When you begin the journey of understanding your fertility, the focus often falls on sperm count, hormones, or lifestyle factors. But there’s a small, tightly coiled structure tucked behind your testicles that plays one of the biggest roles in male fertility: the epididymis.
If you’re reading this because you’re trying to conceive or looking for answers about unexplained male-factor infertility, learning about the epididymis can bring clarity and direction. Understanding how it works—and how things can go wrong—can help you take informed steps toward treatment and hope

Free Thursday Consultation
Book Your AppointmentWhat Is the Epididymis and Why Does It Matter?
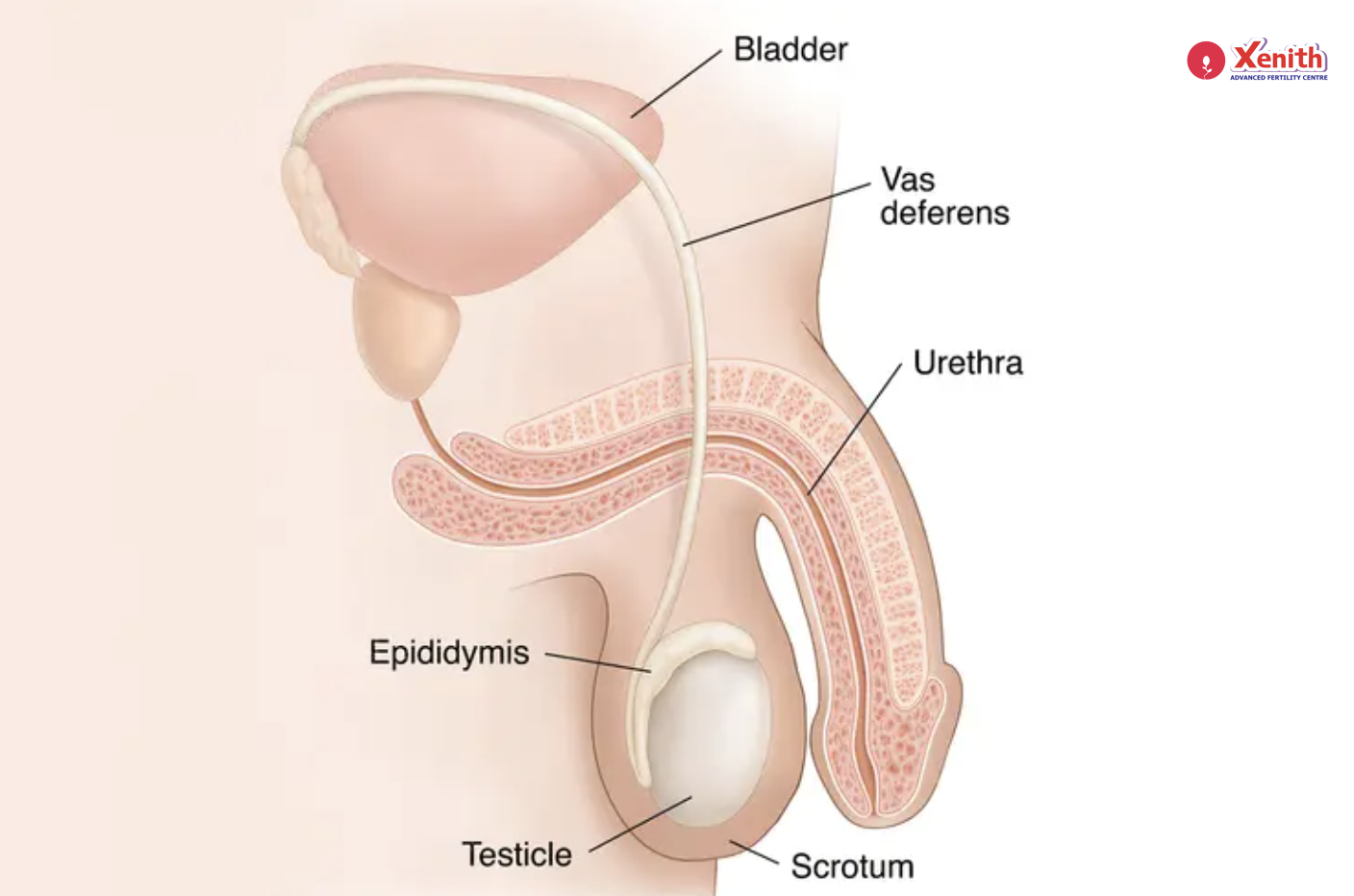
The epididymis is a soft, curved tube that sits on the back of each testicle. Think of it as the body’s natural “finishing school” for sperm. After sperm are produced in the testes, they are immature and unable to swim. They enter the epididymis, where over several days they undergo crucial maturation.
Inside this long, coiled tube, sperm gain motility, the ability to swim, and the capacity to fertilize an egg. The epididymis also stores sperm until ejaculation. Any abnormality in this structure—whether blockage, inflammation, or developmental issues—can disrupt sperm transport and significantly affect fertility.
Common Epididymal Abnormalities and How They Impact Fertility
Understanding the different types of epididymal conditions helps you see how they might affect your ability to conceive.
1. Epididymal Obstruction
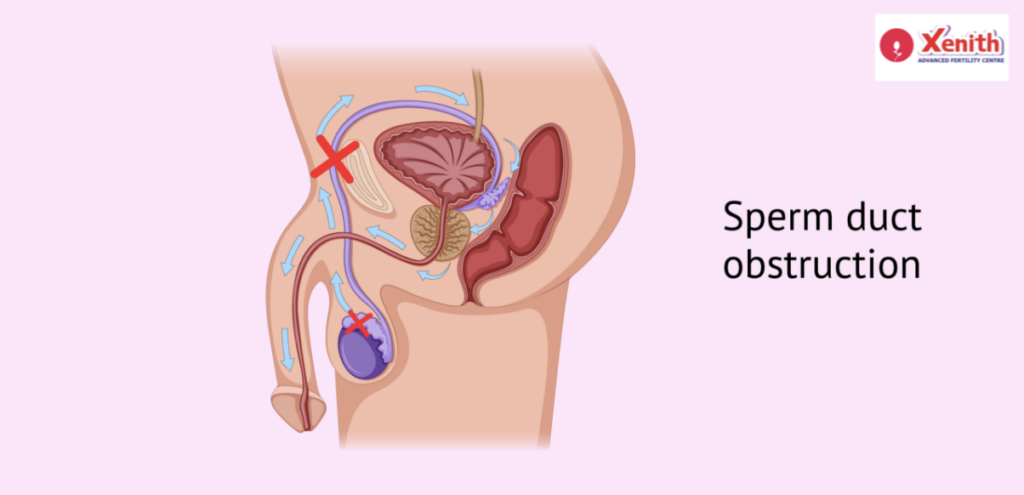
Epididymal obstruction is one of the most common male infertility causes related to this structure. A blockage anywhere within the epididymal tubules can prevent sperm from moving from the testes into the vas deferens.
How it affects fertility
- Sperm production in the testes is usually normal.
- But sperm cannot exit the epididymis, leading to:
- Azoospermia (no sperm in semen)
- Sometimes, epididymal congestion, where pressure builds up behind the blockage
- This congestion may cause discomfort or swelling.
You might not feel any symptoms at all—many men discover the issue only when they see a low or zero sperm count in a semen analysis.
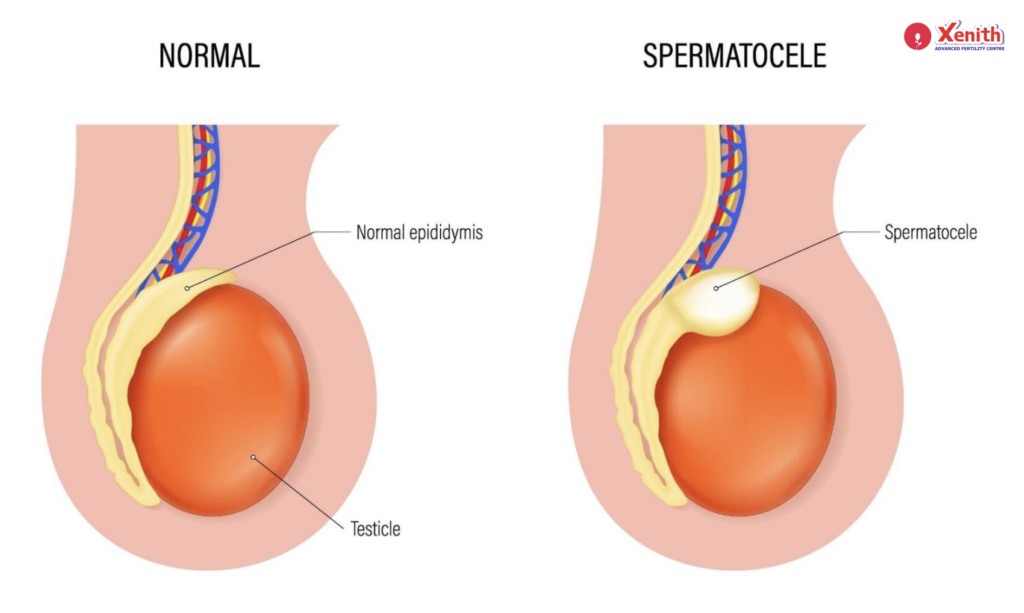
2. Epididymal Cysts
Epididymal cysts are fluid-filled sacs that develop in or around the epididymis. These are often benign and common.
How they affect fertility
Most epididymal cysts do not impact fertility unless they are unusually large or physically compress the sperm-carrying ducts. When they do interfere, they may cause:
- Blockage of sperm transport
- Discomfort or heaviness in the scrotum
- Occasionally tenderness
If you’ve noticed a lump near your testicle, it can understandably be worrying—but most cysts are harmless and manageable with simple monitoring.
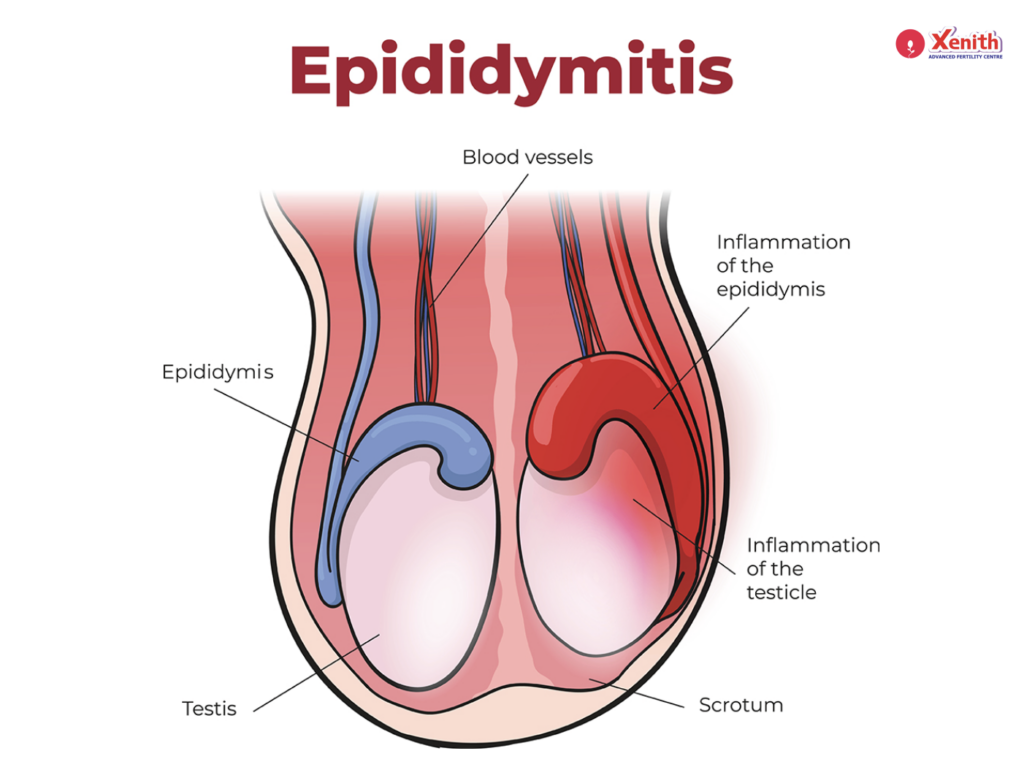
3. Inflammation: Epididymitis
Epididymitis refers to inflammation of the epididymis, often caused by infections. In younger men, sexually transmitted infections (STIs) are common causes, while urinary tract infections and prostate issues are more typical in older men.
How it affects fertility
Inflammation can:
- Narrow or block the epididymal tubules
- Damage the delicate lining where sperm mature
- Reduce sperm health and motility
If untreated, chronic inflammation may lead to scarring and long-term obstruction.
Symptoms may include:
- Pain or tenderness in the scrotum
- Swelling
- Redness or warmth
- Fever (in infectious cases)
- Pain during ejaculation
Early treatment is key to preventing long-term damage.
4. Congenital Absence of the Epididymis
In rare cases, a man may be born without part or all of the epididymis. Sometimes this occurs along with the absence of the vas deferens (as seen in certain genetic conditions like cystic fibrosis carriers).
How it affects fertility
Without an epididymis, sperm cannot mature or travel out of the testes. These men often have:
- Azoospermia
- Normal testosterone and sexual function
- No pain or visible symptoms
This condition typically requires assisted reproductive techniques for conception.
How Epididymal Abnormalities Affect Sperm and Fertility
Regardless of the specific condition, most epididymal abnormalities affect fertility in one central way: they interfere with the movement and maturation of sperm.
Here’s how that plays out:
- Sperm may be produced normally in the testes.
- But if the epididymis is blocked, inflamed, or missing, sperm cannot travel onward.
- Inflammation or cysts may also alter the epididymal environment, affecting sperm quality.
This means that your semen analysis may show:
- Low sperm count (oligospermia)
- Poor motility
- Absent sperm (azoospermia)
- Normal semen volume but no sperm
Many men are surprised to learn that infertility may be their only symptom, especially in silent conditions like epididymal obstruction or congenital absence.
Diagnosis: How Doctors Identify the Problem
If you’re undergoing evaluation for infertility, the diagnostic process can feel overwhelming. But each test offers valuable information to pinpoint what’s happening.
1. Semen Analysis
This is usually the first step. It can reveal:
- Low or absent sperm count
- Poor motility
- Signs of blockage (e.g., normal volume but no sperm)
A pattern of azoospermia with normal hormonal levels often points toward an obstruction in the epididymis.
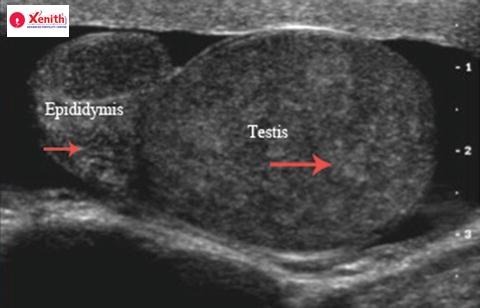
2. Scrotal Ultrasound
A scrotal ultrasound is painless and provides a clear image of the:
- Epididymis
- Testes
- Any cysts or swelling
- Evidence of obstruction or inflammation
It can detect cysts, structural abnormalities, and signs of epididymal congestion.
3. Physical Examination
Your urologist will gently examine the scrotum to check for:
- Tenderness
- Swelling
- Cysts
- Dilated structures
- Absence of vas deferens (which may hint at congenital issues)
This hands-on evaluation can provide immediate clues and guide further testing.
Treatment Options: What You Can Do
The good news is that many epididymal abnormalities are treatable. Even when natural conception isn’t possible, assisted reproductive technologies can offer excellent chances of parenthood.
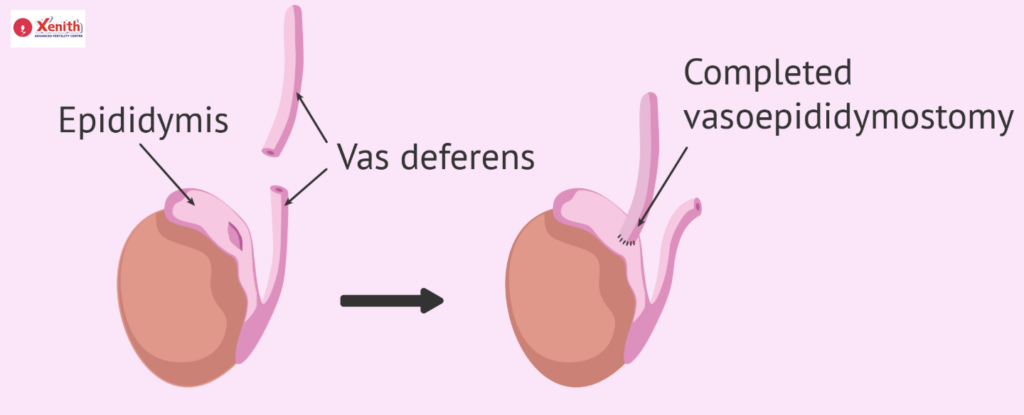
1. Surgical Correction
When a blockage is found, microsurgical procedures may help:
- Epididymovasostomy (connecting the epididymis directly to the vas deferens)
- Vasoepididymostomy (a similar technique depending on obstruction location)
2. Treating Infections and Inflammation
For epididymitis caused by infection, treatment may include:
- Antibiotics
- Anti-inflammatory medication
- Scrotal support and rest
Early treatment protects the epididymis from long-term scarring.
3. Sperm Retrieval for IVF/ICSI
If surgery isn’t possible or successful, sperm can often be retrieved directly from the testes or epididymis using techniques such as:
- PESA (Percutaneous Epididymal Sperm Aspiration)
- TESA (Testicular Sperm Aspiration)
- MESA (Microsurgical Epididymal Sperm Aspiration)
These retrieved sperm are then used in IVF/ICSI, giving couples a strong chance of conception.
Lifestyle & Prevention Tips
While not all epididymal issues are preventable, you can reduce your risk with a few targeted habits:
1. Prevent Infections
- Practice safe sex
- Seek early treatment for urinary or reproductive infections
- Get screened if you’re at risk for STIs
2. Protect Against Trauma
- Wear protective gear during contact sports
- Avoid prolonged pressure on the groin area
3. Manage Heat Exposure
- Avoid long hours in hot tubs or saunas
- Do not keep laptops on your lap for extended periods
4. Address General Health
- Manage chronic conditions such as diabetes
- Maintain a healthy weight
- Avoid smoking and excessive alcohol
These habits support not only epididymal health but overall sperm quality.
Conclusion:
Facing the possibility of an epididymal abnormality can be unsettling, especially when you’ve been trying to conceive. But understanding the role of the epididymis empowers you to make informed decisions. With modern diagnostic tools, surgical options, and assisted reproductive techniques like IVF/ICSI, most couples find a path that works for them.
You’re not alone on this journey. With the right medical guidance, lifestyle choices, and support, there is real hope—and real help—available. If you suspect an epididymal condition or have been struggling with fertility, reaching out to a qualified urologist or fertility specialist can be the first step toward clarity, healing, and the future you’re hoping for.