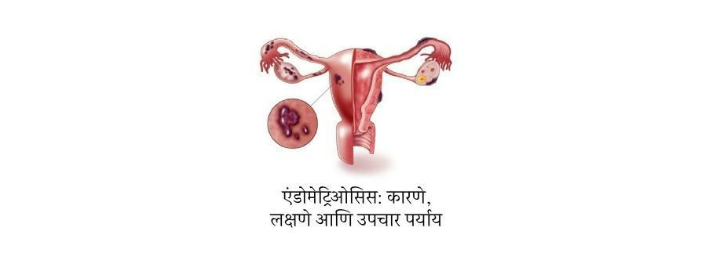
एंडोमेट्रिओसिस: कारणे, लक्षणे आणि उपचार पर्याय
महिलांचे आरोग्य हा एक महत्त्वाचा विषय आहे ज्याबाबत अधिक जागरूकता आणि समज आवश्यक आहे. अशीच एक आरोग्य समस्या म्हणजे एंडोमेट्रिओसिस, जी जगभरातील लाखो महिलांना प्रभावित करते. ही समस्या सामान्य असूनही, ती अनेकदा चुकीची निदान केली जाते किंवा दुर्लक्षित केली जाते.…