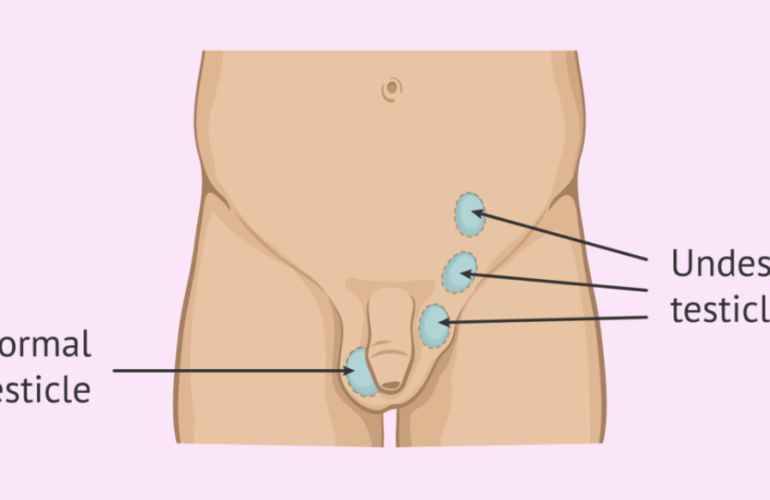
Testicles are located in the scrotum which Is a loose bag of skin under the penis. Sperm is produced in the testicles and male hormones like testosterone are also made here. Cancer is a disease where some cells begin to grow and multiply uncontrollably eventually spreading to other areas of the body. Testicular cancer is cancer of the testicles.
How does it affect fertility

Free Thursday Consultation
Book Your AppointmentOften, testicular cancer will occur in one testicle and the unaffected testicle could make enough testosterone and sperm. Almost all testicular cancers start in the germ cells in the testicles which make sperm and thus the cancer itself and its treatment could affect fertility. Sometimes treatment might involve removing the testicle which is needed for reproduction and some treatment might affect some hormone levels and might damage the DNA in the sperm itself leading to issues with infertility or might even cause miscarriages or birth defects in the baby. After chemo treatment, the production of sperm might slow down or might stop completely. It might take a few years for sperm production to return and sometimes it might not be produced at all.
So, make sure to discuss with your doctor how to preserve your fertility if you have plans to have children in the future before you begin treatment. Fertility could also depend on your age, other health issues, the severity of the cancer, and the type of treatment.
What causes testicular cancer
It’s most common in young men. There is a higher risk of testicular cancer if there is a family history of it, if you have had testicular cancer before or if you are born with certain congenital malformations of the genitals. (1, 2) Some environmental factors could also cause testicular cancer. Most testicular cancers can be cured even if it’s found at an advanced stage.
Symptoms
Most testicular cancers can be detected early although in some cases there may be no symptoms until the advanced stage. Often, a lump in your testicle could be the first sign of the testicle could be swollen. Other symptoms could include pain in the testicle or scrotum, feeling of heaviness in the scrotum or lower abdomen, low back pain, or breast growth/soreness. It’s often normal that one testicle is larger than the other or that one hangs lower than the other. So, it is recommended that you should examine their testicles routinely.
Diagnosis
Blood tests might be done to look for certain proteins called tumor markers or other enzymes which could indicate the presence of a tumor or cancer in the testicles. An ultrasound could be done to verify the presence of a cancerous tumor or benign (noncancerous) tumor or if it’s some other condition like a varicocele (varicose veins in the scrotum) or something else. Another diagnostic tool could be surgery although getting a biopsy (small piece of the tumor) is rarely done to prevent the cancer from spreading. Surgery might be done to remove the entire testicle. If testicular cancer has been diagnosed, more tests like CT, MRI and x-ray may be done to see if the cancer has spread to other areas of the body.
Treatment
Treatment may depend on the severity of the cancer. The various treatment options are surgery, radiation therapy, chemotherapy, and other new treatment undergoing clinical trials. Surgery is done to remove the affected testicle and some lymph nodes where the cancer might have spread as well as any tumors. After the surgery, you might need to undergo chemotherapy and/or radiation therapy to make sure any remaining cancer cells are destroyed. Radiation therapy uses X-ray or other types of radiation to kill cancer cells. If radiation is directed at one testicle, the other testicle should be shielded with a lead shield if possible. Chemotherapy uses drugs to kill the cancer cells or stop them from dividing. Since sperm cells also divide quickly, they could also be damaged by chemotherapy. After the treatment has ended, follow up tests might be done to make sure cancer is in remission and doesn’t come back.
Ways to preserve your fertility
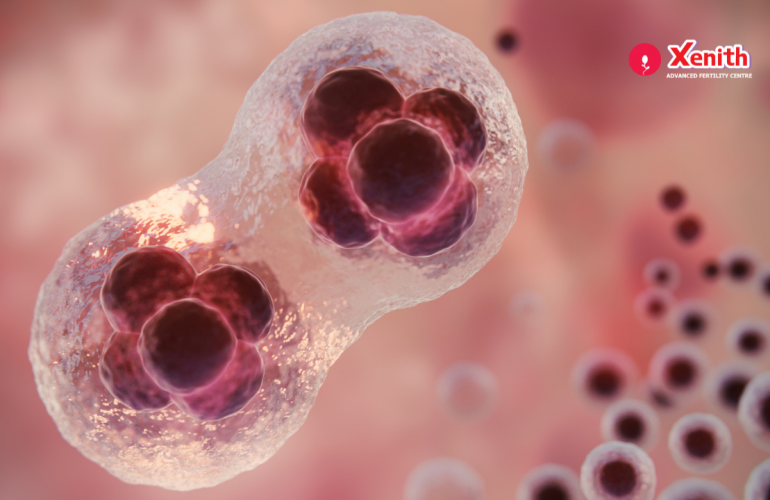
Fertility preservation might be needed to save the sperm for future use if you are diagnosed with testicular cancer and it should be done as soon as possible. It may involve storing your sperm in a sperm bank for future use. Here, the sperm in the semen sample is tested for quality, quantity, motility as well as other parameters and then cryopreserved (frozen) and stored. The process of cryopreservation involves separating the sperm from the semen, placing it in a special freezing solution and frozen in liquid nitrogen at -196oC. This prevents ice crystal formation which can damage the sperm. However, some sperm banks will not accept semen samples that are positive for some infectious diseases like HIV or hepatitis. The samples will be viable for a long time. In the future, the frozen sperm can then be thawed and used for conception in the future via intrauterine insemination (IUI) or in vitro fertilization (IVF) together with intracytoplasmic sperm injection (ICSI). IUI is a procedure where the sperm is transferred to the woman’s uterus when she is ovulating in order to conceive. IVF is a procedure where the woman’s eggs are retrieved from her ovaries, and placed with many sperm in a laboratory setting in order for fertilization to occur and form an embryo which is then transferred back to the woman’s uterus for conception to occur. Sometimes in the case of severe male infertility, a single sperm is injected into an egg for fertilization to occur and this process is called ICSI.
Cancer can take a toll on your body physically but it could also affect you mentally and emotionally. You might feel your life has been turned upside down and may feel overwhelmed with all the information and new terminology presented from your doctor. You may feel angry, afraid, worried, guilty and ask yourself constantly why this would happen to you. You may distance yourself from others to figure out what to do or you may feel very lonely. You may also know others who have had cancer and survived and have some hope. It could also lead to stress, anxiety and depression. After the treatment is finished you might also have to adjust to a “new normal” being careful of everything you do, being scared of the cancer recurring and for going back for a check up. (4) So how do you cope with all this? It might help to have someone close to talk to and air out your feelings and concerns whether it be your close friend, your spouse, a support group or a counsellor. It may help to not blame yourself and try to see the positive side of things. Try to do things that relax you like listening to music, going for a walk, doing yoga and meditating, journaling, painting, going for a massage or trying out a new hobby. If you are dealing with depression, you might need to see a professional. You might also find peace in your faith. Just know that testicular cancer has a high survival rate and it can be beaten. So take a few deep breaths and stay positive. If you wish to speak to some professional about how testicular cancer could affect your fertility, come talk to us at Xenith Advanced Fertility Centre.