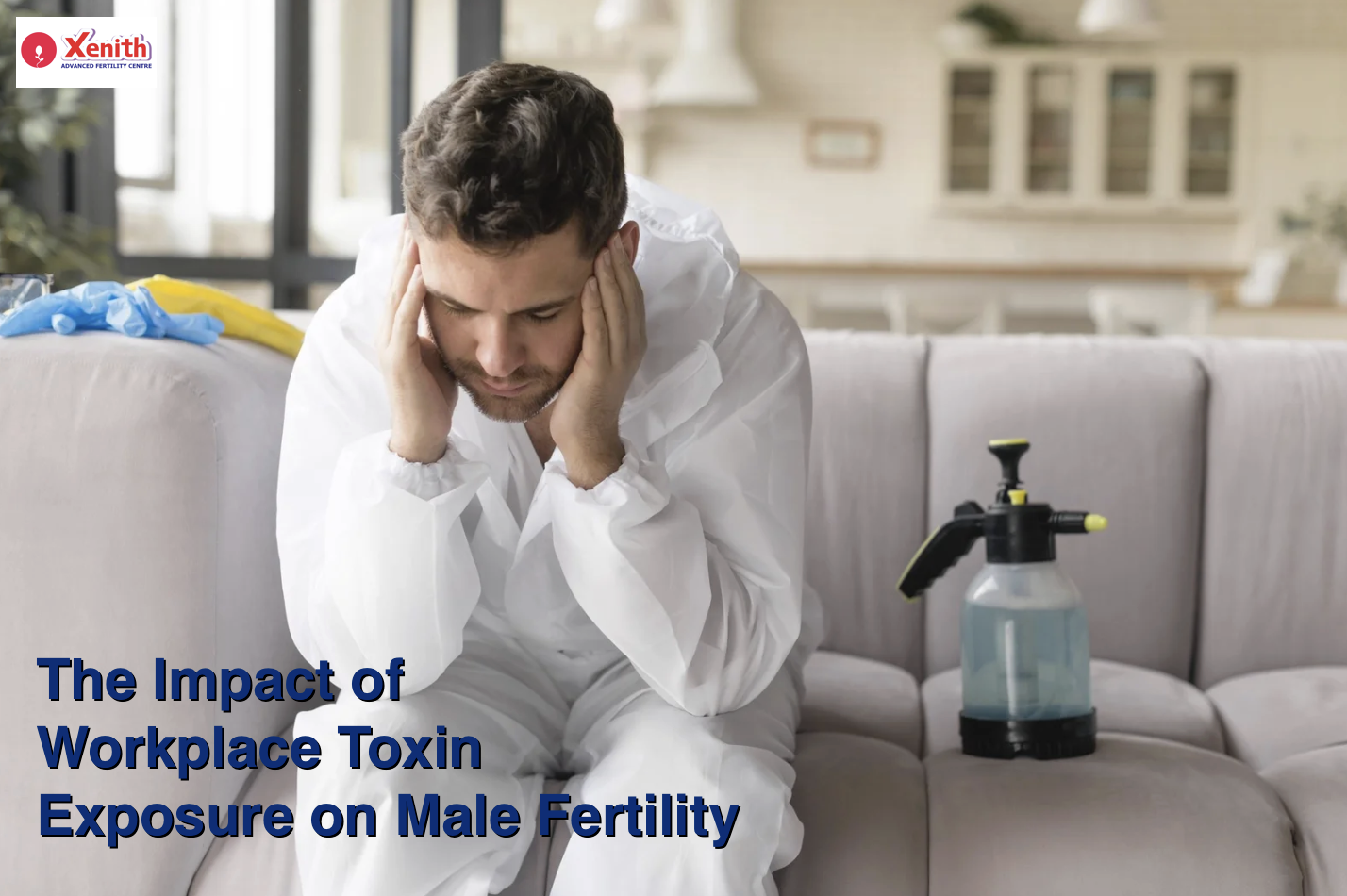
Introduction: How Your Work Environment Could Be Affecting Your Fertility
In today’s world, conversations around fertility often focus on diet, lifestyle, and age—but there’s another, often overlooked factor that could quietly be affecting your reproductive health: toxin exposure at the workplace.
You might not realize it, but the chemicals, fumes, or materials you’re exposed to during your workday can have a significant impact on your overall health—including your fertility. As awareness grows around how environmental factors influence reproductive wellbeing, it’s crucial to understand how workplace toxins can affect you and what steps you can take to protect yourself.

Free Thursday Consultation
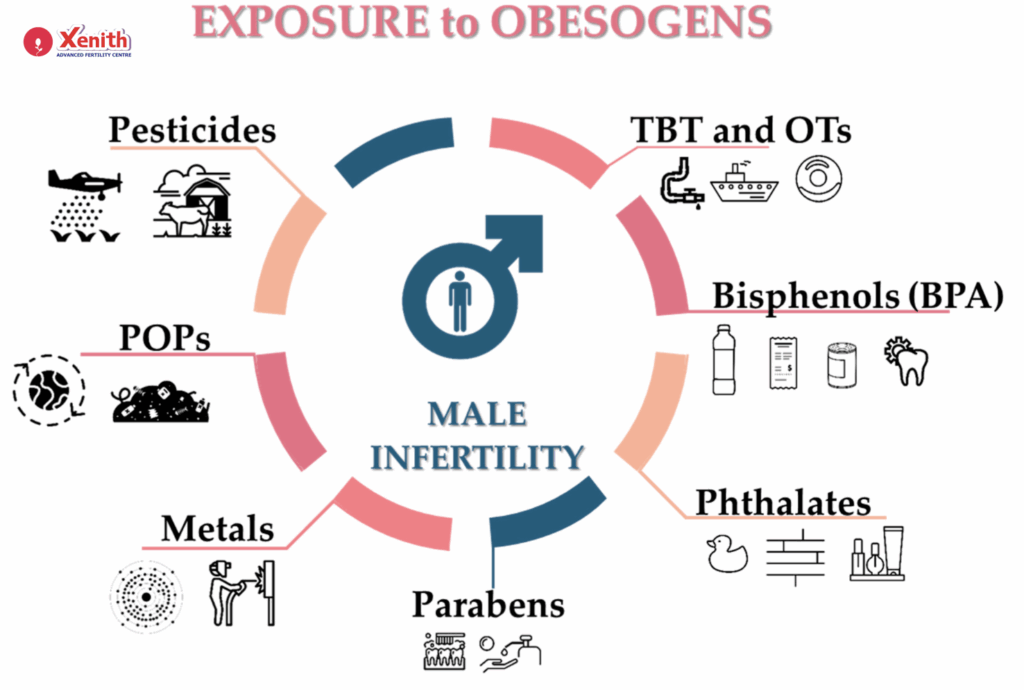
Book Your AppointmentWorkplace toxins include a wide range of substances—from pesticides and solvents to heavy metals and radiation. These aren’t just industrial hazards; they can also be found in healthcare, construction, manufacturing, and even office environments. Over time, consistent exposure to these toxins can disrupt hormonal balance, impair sperm health, and increase the risk of infertility.
Common Workplace Toxins and Their Effects on Sperm Health
Several substances commonly encountered at work have been shown to affect male fertility. Here are some of the major ones:
- Pesticides: Commonly used in agriculture, pesticides can interfere with testosterone production and reduce sperm count.
- Heavy metals like lead, cadmium, and mercury can affect sperm motility (movement) and morphology (shape), making it harder for sperm to fertilize an egg.
- Solvents and chemicals found in cleaning agents, paints, or industrial materials can alter sperm DNA, leading to higher rates of DNA fragmentation.
- Radiation—whether from X-rays, electronic equipment, or other sources—can damage the genetic integrity of sperm.
When sperm DNA gets damaged, it doesn’t just affect fertility—it can also increase the risk of miscarriages or developmental issues in offspring. These changes might not show up immediately, which is why consistent awareness and preventive measures are so important.
Occupations at High Risk of Toxin Exposure
Certain jobs naturally carry a higher risk of exposure to harmful substances:
- Agriculture: Regular contact with pesticides, fertilizers, and herbicides can severely impact sperm quality.
- Construction and painting: Workers often deal with solvents, dust, heavy metals, and asbestos.
- Manufacturing and industrial work: Exposure to chemicals like benzene, phthalates, or plasticizers can interfere with hormone production.
- Healthcare: Medical professionals may be exposed to radiation, anesthetic gases, and disinfectants.
If you work in any of these fields, taking extra precautions isn’t just about physical safety—it’s also about protecting your reproductive health and your family’s future.
The Science Behind Toxin Exposure and Infertility
So, how exactly do toxins affect fertility? The answer lies in the way they disrupt your body’s delicate hormonal and cellular balance.
Many workplace toxins act as endocrine disruptors, which means they interfere with hormones like testosterone that are essential for sperm production. They may either mimic natural hormones or block their effects, leading to reduced sperm output or abnormal development.
Toxins can also trigger oxidative stress, a condition where the body produces excessive free radicals—unstable molecules that damage cells, including sperm cells. Since sperm are highly sensitive to oxidative damage, this can result in lower motility, abnormal shapes, and DNA damage.

Over time, such disruptions can lead to decreased fertility and longer conception times—even if you appear healthy otherwise.
Preventive Measures and Protective Gear
The good news? You can take concrete steps to minimize exposure and safeguard your fertility.
Start by using personal protective equipment (PPE) such as gloves, respirators, masks, and protective clothing. These barriers significantly reduce direct contact and inhalation of harmful substances.
Workplace ventilation and air filtration systems also play a vital role. If you work in enclosed or poorly ventilated spaces, make sure proper airflow and exhaust systems are in place to minimize airborne toxins.
Lastly, always follow safety protocols and occupational guidelines. Many workplaces have standard operating procedures (SOPs) designed to reduce exposure—make sure you’re not cutting corners when it comes to your health.
Detoxification Strategies and Lifestyle Changes
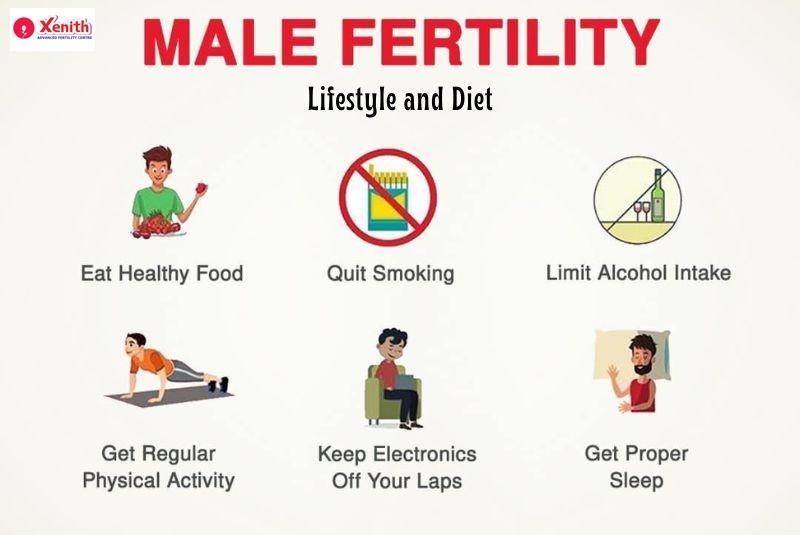
Even with the best precautions, some exposure may still occur. Supporting your body’s natural detoxification processes can make a big difference.
- Eat antioxidant-rich foods like berries, leafy greens, nuts, seeds, and green tea. Antioxidants help neutralize free radicals and repair cellular damage.
- Stay hydrated to help flush out toxins through your liver and kidneys.
- Exercise regularly to improve circulation, support hormonal balance, and reduce oxidative stress.
- Avoid smoking and limit alcohol intake, as both can worsen toxin-induced sperm damage.
These small, consistent lifestyle changes can go a long way in maintaining your reproductive health—even if your work environment poses challenges.
Legal Rights and Workplace Safety Regulations
You have a right to a safe working environment. In most countries, laws and regulatory bodies like OSHA (Occupational Safety and Health Administration) or equivalent national agencies ensure that workplaces follow safety standards to protect workers from harmful exposure.
If you suspect unsafe conditions or feel your health is being compromised, you have the right to report it without fear of retaliation. Employers are legally obligated to provide protective gear, training, and proper waste disposal systems to minimize risk.
Being informed about your rights empowers you to demand the safety you deserve.
Seeking Medical Advice and Fertility Testing
If you work in a high-risk occupation or have been exposed to toxins over a long period, consider getting regular fertility check-ups.
A semen analysis can give insights into your sperm count, motility, and morphology, while hormone evaluations can reveal imbalances that might be affecting fertility.
If abnormalities are detected, a fertility specialist can recommend treatments or lifestyle interventions. In some cases, assisted reproductive technologies (like ICSI or IVF) can help overcome sperm-related issues caused by toxin exposure.
It’s always better to get checked early—especially if you’ve been trying to conceive for more than six months without success.
Conclusion: Protecting Your Fertility at Work
Your job might be your livelihood, but your health is your foundation. Protecting yourself from workplace toxins isn’t just about avoiding immediate illness—it’s about safeguarding your fertility, your hormones, and your long-term well-being.
By staying aware, following safety protocols, using protective gear, and maintaining a healthy lifestyle, you can significantly reduce your risk. Don’t wait for symptoms to appear—take proactive steps now to ensure your body stays resilient and capable for years to come.
FAQ
Workplace toxins are harmful chemicals or substances like pesticides, heavy metals, solvents, and radiation. They can lower sperm count, affect sperm motility and shape, and damage sperm DNA.
Agriculture, construction, manufacturing, and healthcare are among the most high-risk professions.
They disrupt hormone production and increase oxidative stress, leading to poor sperm quality and DNA damage.
Oxidative stress occurs when toxins cause an imbalance between free radicals and antioxidants, damaging sperm and reproductive tissues.
Always wear gloves, masks, respirators, and protective clothing—especially when handling chemicals or working in poorly ventilated areas.
They reduce airborne toxin concentrations and prevent inhalation of harmful particles.
Include antioxidant-rich foods, hydrate well, and maintain a balanced diet with fresh fruits and vegetables.
You are entitled to a safe workplace under OSHA and similar regulations. Employers must provide safety gear and proper training.
If you’ve been exposed for several years or are struggling to conceive after six months of trying, it’s time for a semen analysis.
Yes. Treatments like ICSI or IVF can help, but early detection and lifestyle changes remain the best defense.