Assessment
If you’ve been trying to conceive for a while and haven’t had success, it’s natural to start looking for answers. Fertility issues can be emotionally exhausting, but understanding what’s happening inside your body is the first step toward finding a solution. One important diagnostic tool that can help uncover potential causes of infertility is Hysterosalpingography (HSG).
HSG is a special type of X-ray that helps your doctor evaluate your uterus and fallopian tubes. It plays a vital role in identifying any blockages, structural issues, or abnormalities that might be standing in the way of conception. For many women, undergoing an HSG is a crucial step in their fertility journey — providing both clarity and direction for the next course of action.

Free Thursday Consultation
Book Your AppointmentWhat is Hysterosalpingography (HSG)?
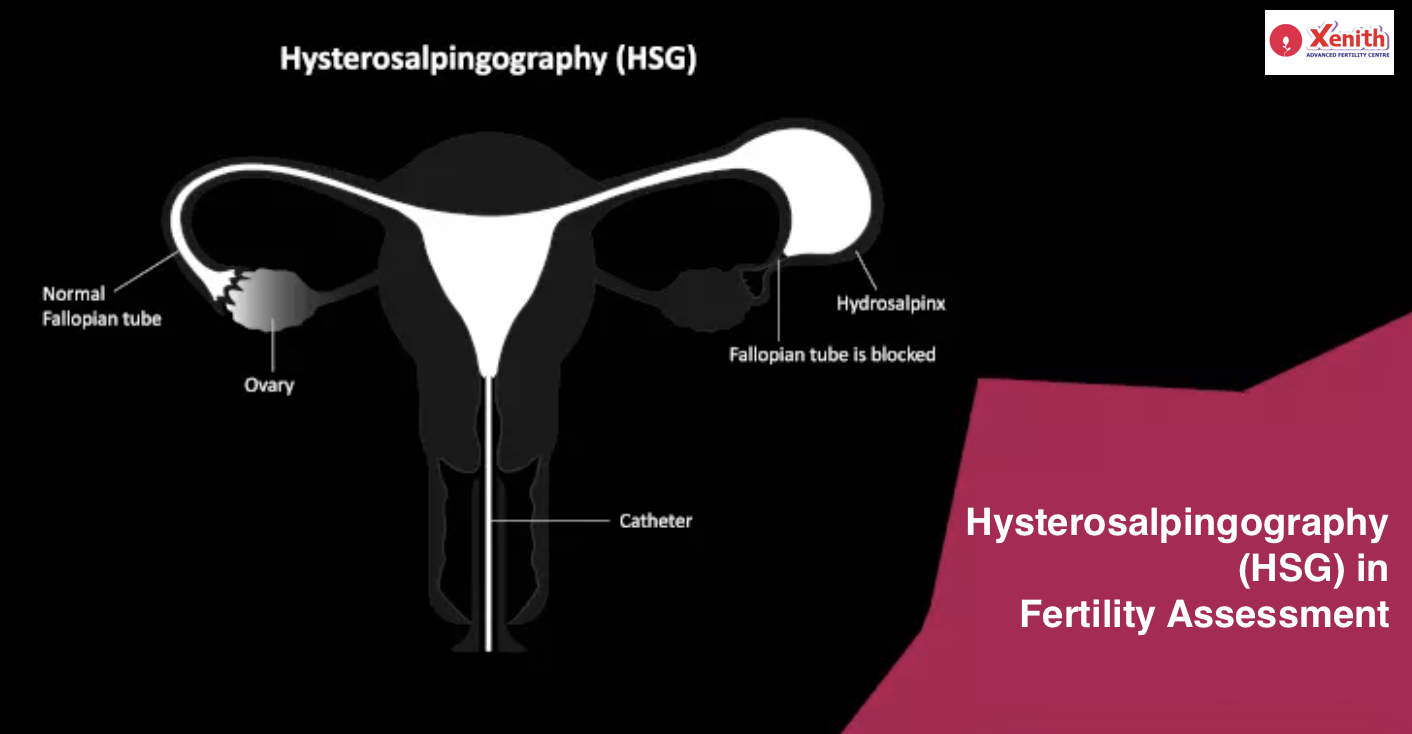
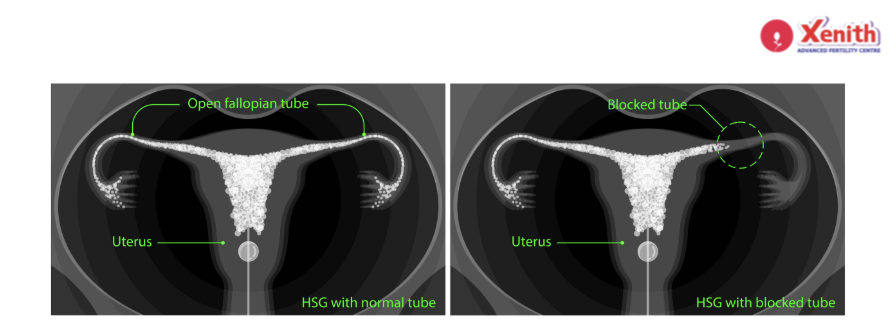
Hysterosalpingography (HSG) is a medical imaging procedure used to assess the shape and structure of the uterus and to check whether the fallopian tubes are open or blocked. These two factors are key to natural conception — because for pregnancy to occur, the egg and sperm need to meet in an open fallopian tube.
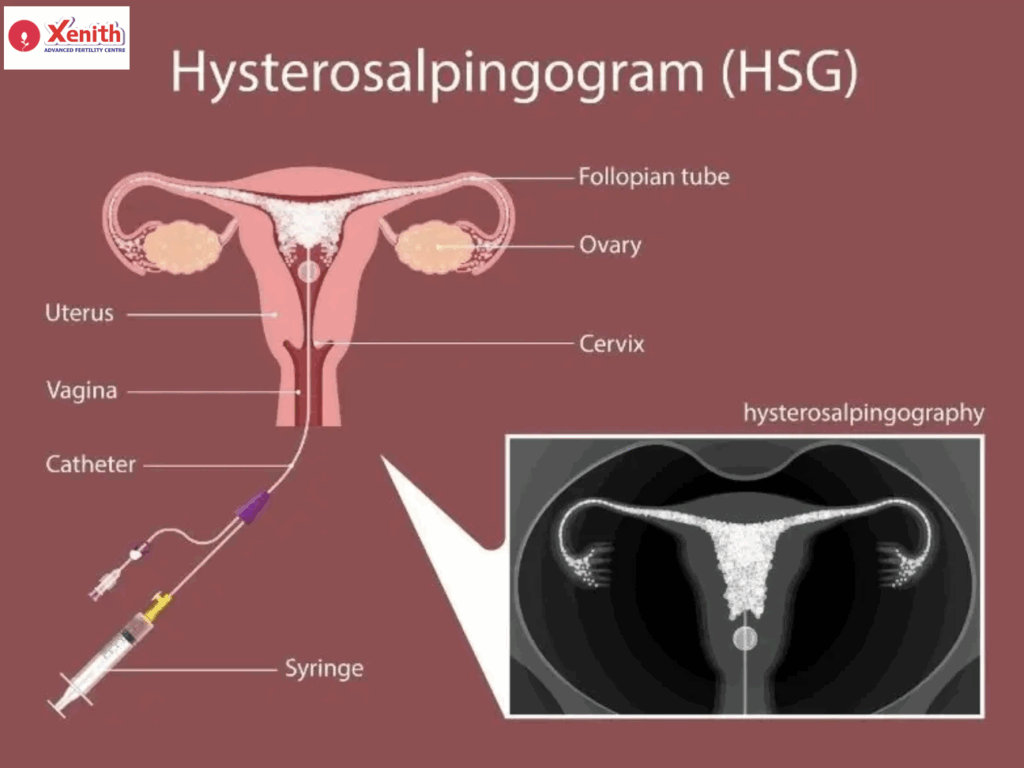
During the procedure, a contrast dye (a special liquid visible under X-ray) is gently introduced through the cervix into the uterus and fallopian tubes. As the dye flows through, a series of X-ray images are taken. These images allow your doctor to see the outline of the uterus and tubes and detect any abnormalities such as blockages, adhesions, or structural issues.
It’s a quick, minimally invasive test that provides valuable information about your reproductive health — and in some cases, it may even improve fertility by flushing out minor blockages.
Why is HSG Important for Fertility Assessment?
When you’re struggling to conceive, there can be many potential reasons — hormonal imbalances, egg quality, ovulation problems, or issues in the uterus and fallopian tubes. HSG specifically focuses on the anatomical aspects of fertility.
Here’s why it’s so important:
- Detecting Blockages: One of the most common findings in an HSG is a blockage in one or both fallopian tubes. Such blockages can prevent sperm from reaching the egg or the fertilized egg from reaching the uterus.
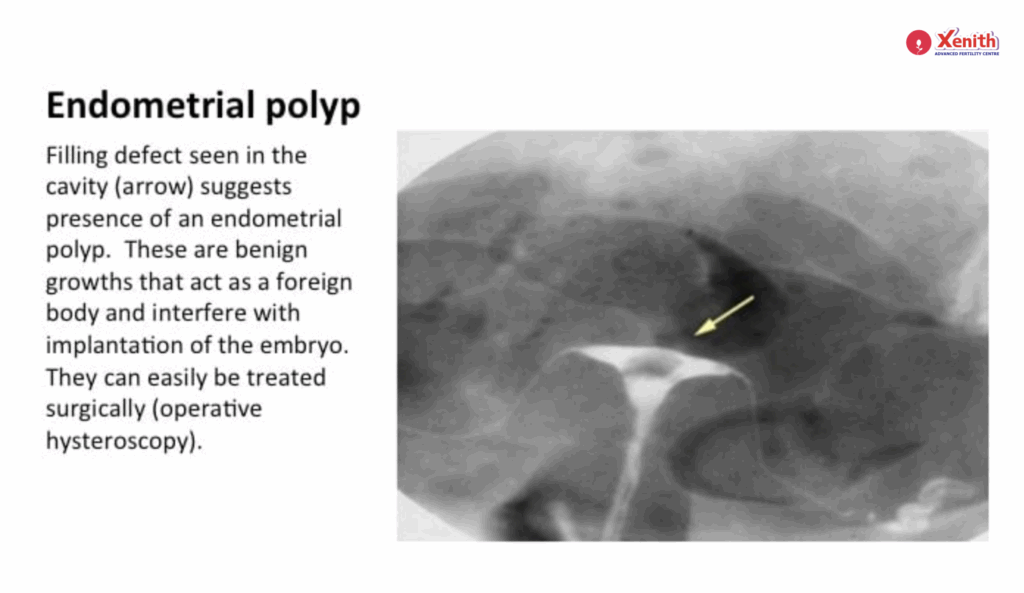
- Evaluating the Uterus: HSG helps visualize the shape and size of your uterus, identifying abnormalities such as fibroids, polyps, or congenital uterine defects.
- Guiding Treatment Plans: The results can guide your doctor to recommend the right treatment — whether it’s surgery to remove a blockage, IVF, or another fertility approach.
- Therapeutic Effect: Interestingly, some women experience an increased chance of conceiving naturally shortly after an HSG. This may be due to the dye flushing out small debris or mucus plugs from the fallopian tubes.
What Conditions Can HSG Detect?
HSG is a powerful diagnostic tool that can detect several reproductive conditions, including:
Blocked Fallopian Tubes: One or both tubes may be obstructed, often due to infection, pelvic inflammatory disease (PID), or endometriosis.
Uterine Fibroids or Polyps: These growths can interfere with implantation or block the tubes.
Adhesions (Scar Tissue): These can form after surgeries or infections, distorting the uterine cavity or blocking the tubes.
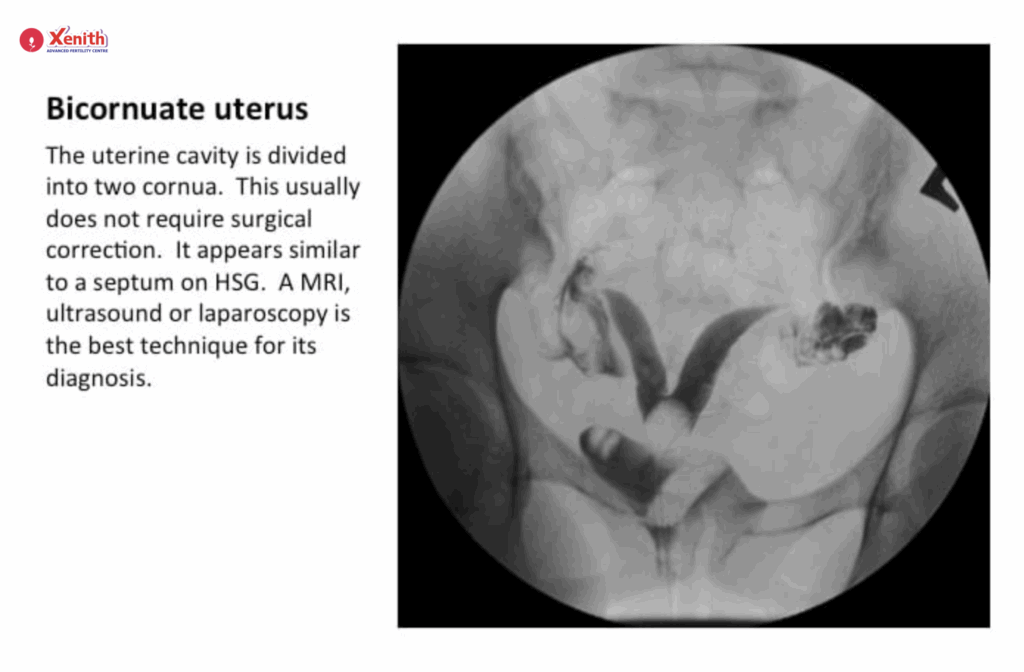
Congenital Uterine Abnormalities: Such as a septate uterus or bicornuate uterus, which can affect fertility or cause recurrent miscarriages.
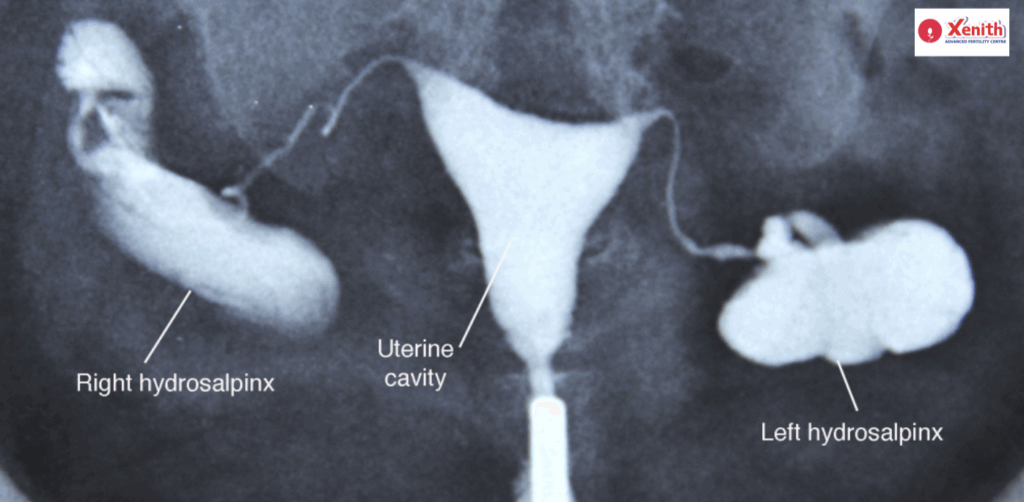
Hydrosalpinx: A condition where a fallopian tube is filled with fluid, often leading to infertility.
The HSG Procedure: Step-by-Step
If your doctor has recommended an HSG, knowing what to expect can help ease anxiety. Here’s a simple breakdown:
1. Before the Procedure:
HSG is usually scheduled after your period but before ovulation (between days 7–10 of your cycle) to ensure you’re not pregnant. You may be advised to take a mild pain reliever or antibiotic before the procedure to prevent discomfort or infection.
2. During the Procedure:
- You’ll lie on an X-ray table, similar to a pelvic exam.
- A speculum is inserted into the vagina to access the cervix.
- A thin tube (catheter) is inserted through the cervix, and the contrast dye is gently introduced.
- As the dye fills your uterus and tubes, X-ray images are taken to track the flow and detect any abnormalities.
- The entire procedure typically lasts 10–20 minutes.
3. After the Procedure:
You may feel mild cramping similar to period pain, and some light spotting may occur. Most women can resume normal activities soon after, but rest is recommended for the remainder of the day.
What to Expect After the HSG Procedure
It’s common to experience:
- Mild abdominal cramps
- Light spotting for a day or two
- Slight dizziness or nausea (rare)
These symptoms usually subside quickly. However, you should contact your doctor if you experience:
- Heavy bleeding
- Fever or chills
- Foul-smelling vaginal discharge
- Severe abdominal pain
These could indicate infection or an allergic reaction to the dye, which is rare but possible.
Interpreting HSG Results
Your doctor will analyze the X-ray images to interpret the findings:
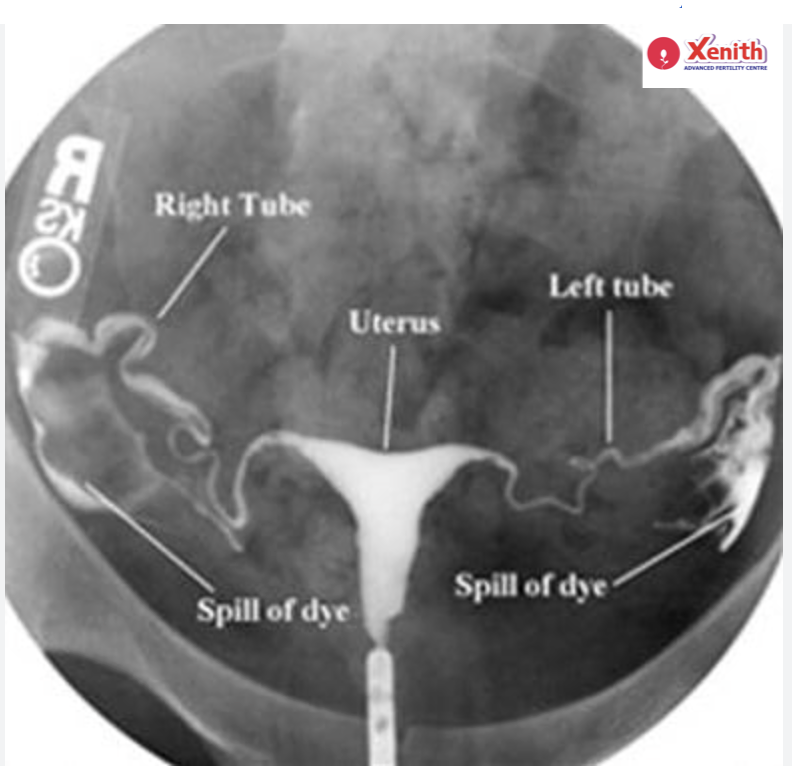
- Normal Results: The dye flows freely through both tubes and spills into the pelvic cavity, indicating open tubes and a normal uterus.
- Abnormal Results: If the dye stops or shows irregularities, it could mean a blockage, fibroid, polyp, or structural issue.
Depending on the results, your doctor may suggest:
- Laparoscopy for further evaluation if there’s a blockage.
- Fertility treatments such as IUI or IVF if both tubes are blocked.
- Surgical correction or medication if fibroids or polyps are detected.
Remember, HSG results are just one part of the overall fertility assessment. Your doctor will combine these findings with other tests (like hormone levels and ovulation tracking) to design the best treatment plan for you.
Conclusion
Hysterosalpingography (HSG) is more than just a test — it’s a window into your reproductive health. It provides essential insights into your uterus and fallopian tubes, helping uncover potential barriers to conception. While the thought of undergoing a medical procedure can be intimidating, HSG is quick, safe, and often provides answers that can bring you closer to your dream of parenthood.
If you’re considering or have been advised to undergo an HSG, talk openly with your fertility specialist. Understanding the purpose, process, and outcomes can help you approach the test with confidence and peace of mind.
FAQ
HSG helps identify structural issues in the uterus and fallopian tubes that might be affecting conception. It’s performed to detect blockages, adhesions, fibroids, or other abnormalities that could hinder pregnancy.
You may feel mild to moderate cramping, similar to menstrual pain, during or shortly after the procedure. The discomfort usually subsides within a few hours. Taking a pain reliever before the test can help minimize this.
The actual imaging part typically lasts 10–15 minutes, though the entire appointment may take about 30–45 minutes including preparation time.
Complications are rare but can include infection, allergic reaction to the dye, or injury to the uterus. Your doctor will take precautions to minimize these risks.
Yes, sometimes! The dye can help flush out small blockages in the fallopian tubes, improving your chances of conception naturally in the months following the procedure.
The best time is after your menstrual bleeding stops and before ovulation — typically between days 7 and 10 of your cycle. This timing ensures you are not pregnant and that the uterus is clear for imaging.
You may be asked to:
1). Avoid intercourse from the start of your period until after the test.
2). Take a mild painkiller about an hour before the procedure.
3). Inform your doctor about any allergies, infections, or possible pregnancy.