Trying to conceive can be an emotional and confusing journey. You may find yourself overwhelmed with advice, cycle tracking apps, and bodily changes that are difficult to interpret. At Xenith Advanced Fertility Centre, we believe that understanding your body’s signals is the first empowering step. That’s why we’ve created this comprehensive, expert-backed guide—to help you tune into your body’s signals and take confident, informed steps toward conception. Learning how to identify ovulation signs gives you more control over timing intercourse and understanding your cycle’s rhythm
What Is Ovulation and Why Do These Symptoms Matter?
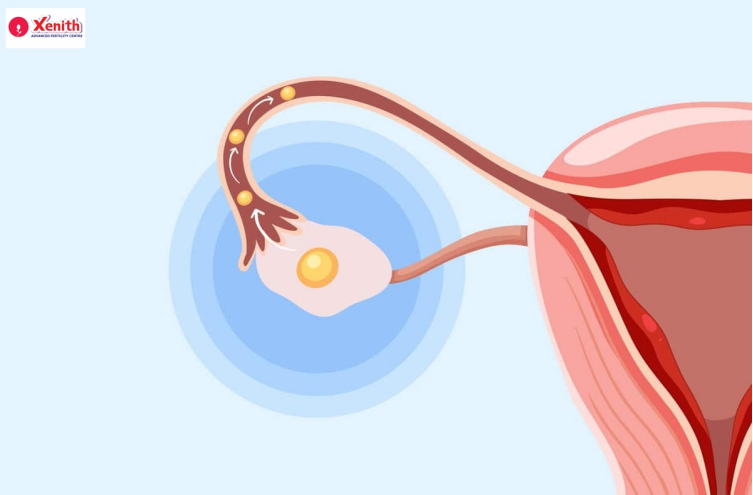
Ovulation is the process when an ovary releases a mature egg, usually around the midpoint of a woman’s menstrual cycle. This ovulation period—typically days 12 to 16 in a 28-day cycle—is your most fertile window. These ovulation symptoms, ranging from physical sensations to subtle changes in your discharge or mood, signal your body’s most fertile period.
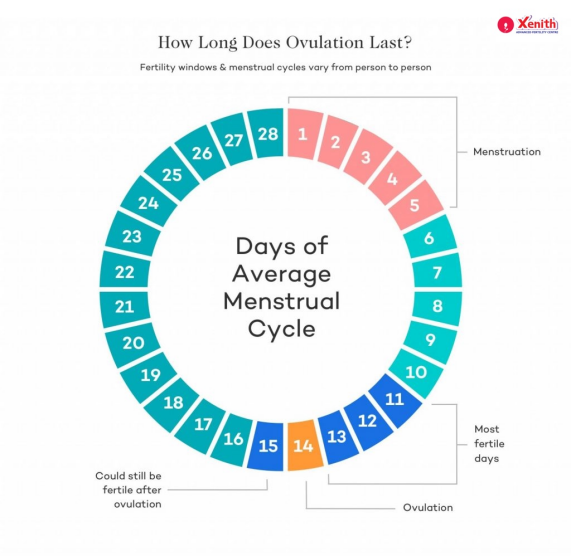
Understanding when ovulation symptoms start and how long your fertile window lasts is important. During your ovulation period, tracking these indicators increases your chances of conceiving naturally.
The 3 Primary Signs of Ovulation: Your Body’s Most Reliable Clues
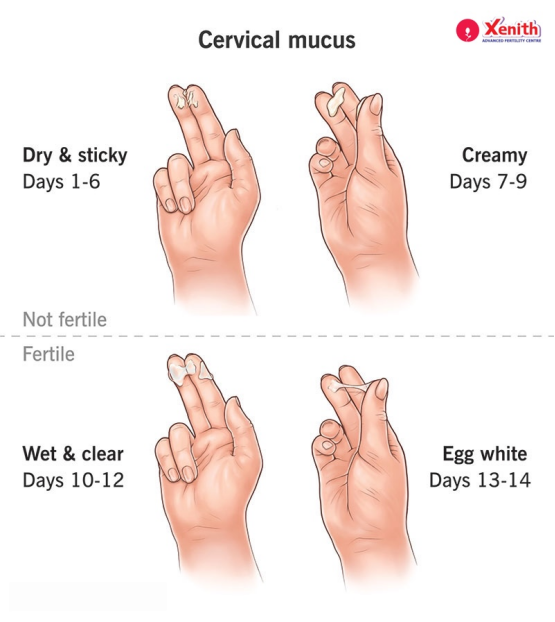
1.Cervical Mucus: A Visual Guide to Your Fertile Window
One of the earliest and most visible signs of ovulation is a change in your cervical mucus. Knowing what ovulation discharge looks like helps identify when you’re most fertile.
Throughout your cycle, mucus changes from:
- Dry (low fertility): Common right after your period; low fertility.
- Sticky or tacky: Early signs of approaching fertility.
- Creamy/lotion-like: Fertile, but not peak.
- Watery: Very fertile.
- Egg white cervical mucus – stretchy, slippery, and clear (like raw egg whites), ideal for sperm movement
User concern:
“My discharge is watery but not really like egg whites. Does that mean I’m not fertile?”
Watery discharge is often a sign that ovulation is near. Not everyone will have textbook egg white mucus, so it’s important to track patterns over time. This method is a key part of learning how to track ovulation symptoms and better understand your own cycle.
2. Basal Body Temperature (BBT): Charting Your Monthly Rhythm
Another reliable method is tracking basal body temperature increase. After ovulation, your temperature rises slightly due to progesterone levels. BBT confirms ovulation after it has occurred. It’s not predictive but helps you understand your cycle better over time
Step-by-step to track BBT:
- Use a basal thermometer.
- Record your temperature first thing in the morning.
- Look for a sustained increase post-ovulation.
User concern:
“My chart is all over the place. What am I doing wrong?”
Sleep disturbances, inconsistent timing, or illness can affect readings. Focus on overall trends rather than individual numbers and try to maintain consistent habits for accurate tracking.
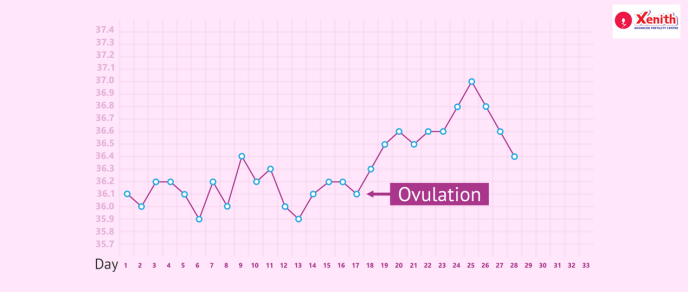
Tracking BBT consistently can also help you answer questions like how many days after ovulation symptoms can you get pregnant, as the temperature rise signals ovulation has occurred.
3.Cervical Position: The High, Soft, and Open Indicator
Checking your cervical position changes during ovulation can give added confirmation. During ovulation, the cervix is:
- High: Difficult to reach
- Soft: Like lips
- Open: Allowing sperm passage
When you’re not fertile, it’s low, firm, and closed.
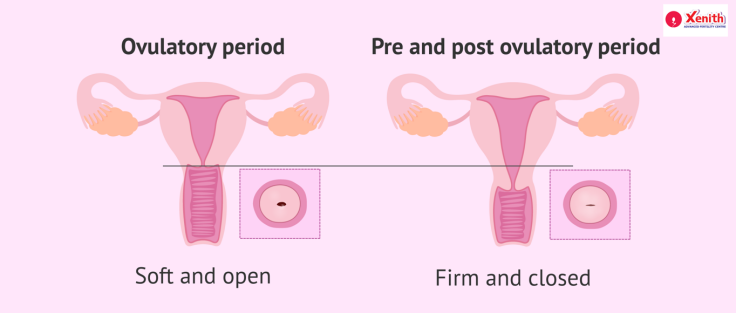
How to check:
- Wash your hands thoroughly.
- Gently insert a clean finger into the vagina.
- Track changes across your cycle for patterns.
This method may take a few cycles to master but is valuable for women wanting a holistic understanding of how to track ovulation symptoms.
Secondary Ovulation Symptoms: Other Clues to Look For
1. Ovulation Pain or ‘Mittelschmerz’: Is It Normal?
Many women experience ovulation pain, also known as Mittelschmerz—a one-sided cramping or discomfort in the lower abdomen. It often occurs right as the follicle releases the egg.
User concern:
“I have cramping—is this normal?”
Mild pain is common, but severe ovulation pain should not be ignored. It could indicate an underlying condition like endometriosis or cysts.

Some may wonder, can you have ovulation pain and not ovulate? The answer is yes—pain does not always indicate egg release, especially if you have hormonal imbalances.
2. Libido, Mood, and More: How Hormones Affect How You Feel
Hormonal changes around ovulation can result in:
- Increased libido
- Mood swings or irritability
- Fatigue
- Heightened sense of smell during ovulation
User concern:
I feel more irritable and anxious around ovulation—is that real?
Absolutely. These hormonal shifts can affect emotional and sensory responses. Everyone reacts differently. Many women report feeling more confident, energetic, and socially open around ovulation—a result of peak oestrogen
3. Other Physical Signs: Spotting, Bloating, and Breast Tenderness
Other lesser-known signs of ovulation include:
- Ovulation spotting vs. period spotting: Light pink or brown discharge mid-cycle
- Ovulation bloating due to fluid retention and hormonal shifts
- Breast tenderness during ovulation caused by estrogen fluctuations
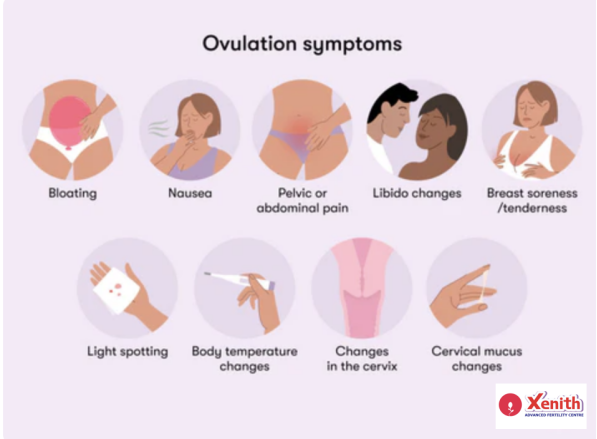
If these signs feel unfamiliar or inconsistent, don’t worry—it’s common to experience no ovulation symptoms occasionally.
How Medical Conditions Like PCOS Can Affect Ovulation Signs
Women with Polycystic Ovary Syndrome (PCOS) often face irregular or absent ovulation. Hormonal imbalances can create ovulation symptoms with PCOS—like mucus changes or bloating—even when ovulation doesn’t occur.
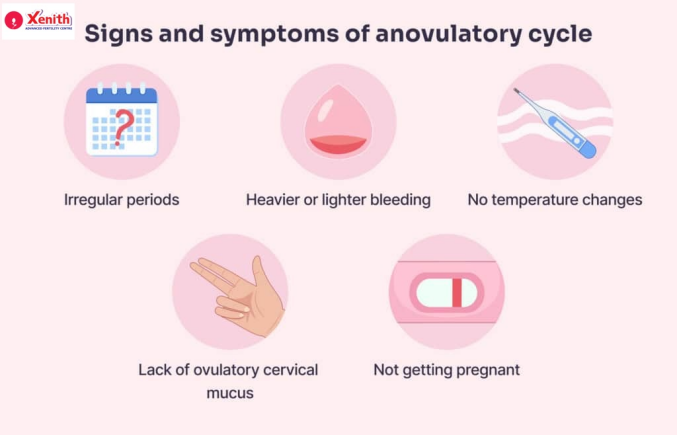
User concern:
“I have PCOS. Can I trust my ovulation signs?”
Unfortunately, symptoms can be misleading with PCOS. In PCOS, LH (luteinizing hormone) levels may be elevated throughout the cycle, causing false positives on ovulation kits. In such cases, follicular monitoring is the most accurate method to detect ovulation. You may also notice why your ovulation symptoms are different this month, which can be due to lifestyle, stress, illness, or underlying hormonal issues.
When Your Symptoms Are Unclear: Next Steps at Out Pune Clinic
Self-tracking has its limits. If you’re confused by your ovulation symptoms or experiencing no ovulation symptoms, you’re not alone. Many try tools like ovulation predictor kits (OPKs) or use an ovulation calculator, but these aren’t foolproof—especially in cases like PCOS.
At Xenith IVF in Pune, we offer:
- Follicular monitoring: Ultrasound-based tracking of your follicles to confirm ovulation
- Hormonal assessments
- Personalized fertility consultations
If you’re tired of second-guessing your body’s signals, a simple follicular study or visit to our fertility clinic in Pune can give you the clarity and support you deserve. Book your consultation at Xenith IVF today.
Conclusion: Your Body Is Your Best Guide
Tuning in to your ovulation symptoms—from discharge and temperature to mood and sensation—gives you powerful insight into your reproductive health.
Whether you’re just beginning or have been trying to conceive for a while, remember: every body is different, and expert guidance can make all the difference.
Whether you are just starting your journey or have been trying for a while, the team at Xenith Advanced Fertility Centre is here to support you with expert guidance and compassionate care. Book your free consultation with our Pune specialists today.
FAQs
1. Can I have ovulation symptoms but not actually release an egg?
Yes. This is common in women with PCOS or stress-related cycle disruptions.
2. How soon after seeing “egg white” mucus should we have sex?
EWCM signals peak fertility. Try to have intercourse within 12–24 hours.
3. Why don’t I experience ovulation pain? Does it mean I’m not ovulating?
Not at all. Many women ovulate without noticeable pain.
4. Can you have symptoms but still have poor egg quality?
Yes. Ovulation symptoms reflect timing, not egg health. Egg quality depends on age, lifestyle, and genetics.
5. Why are my ovulation symptoms different this month?
Stress, diet changes, illness, or travel can all cause your symptoms to vary from cycle to cycle.