Implantation Failure (RIF)
A failed IVF cycle is devastating. But when it happens repeatedly—especially after being told your embryos look “perfect”—it can feel utterly hopeless. You might start wondering if your body is incapable of pregnancy, or if you’ll ever hold your baby.
If this sounds familiar, you’re not alone. Many women face the heartbreak of multiple failed transfers despite transferring good-quality embryos. This condition is known as Recurrent Implantation Failure (RIF)—when a clinical pregnancy isn’t achieved after transferring at least two or three high-quality embryos.

Free Thursday Consultation
Book Your AppointmentThis guide aims to help you move from “Why is this happening?” to “What can I do next?” By understanding the possible causes and the right diagnostic steps, you can take back some control and work toward a personalized, hopeful plan.
Part 1: The “Why” — The 3 Main Causes of Implantation Failure
Think of implantation as a delicate dance between the embryo (the seed), the uterus (the soil), and the body’s internal environment (the climate). When implantation fails repeatedly, the goal is to understand which part of this ecosystem is out of sync.
1. Embryonic Factors (The “Seed”)
Even the best-looking embryos can hide unseen genetic issues. These “aneuploid” embryos have an abnormal number of chromosomes, which makes them incapable of forming a healthy pregnancy—no matter how perfect they look under a microscope.
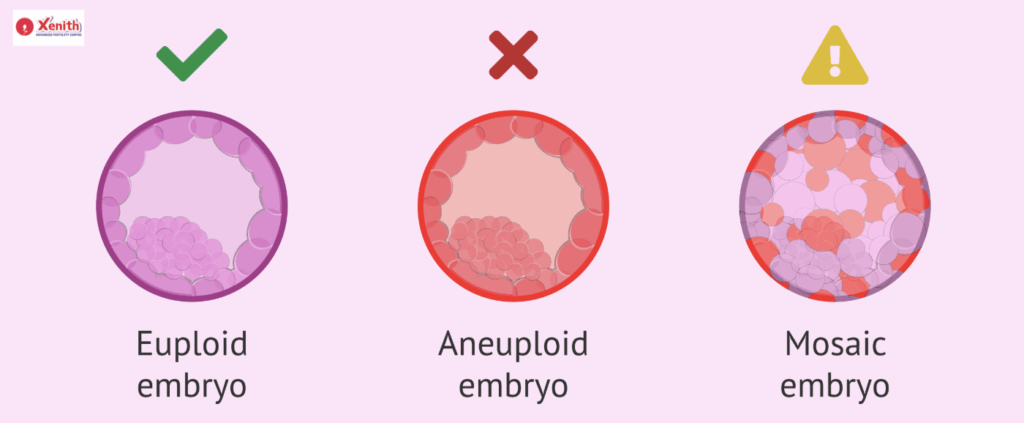
This is where PGT-A (Preimplantation Genetic Testing for Aneuploidy) comes in. PGT-A tests embryos before transfer to identify which ones are “euploid,” or genetically normal. Transferring euploid embryos increases the chances of implantation success.But you may ask, “If my embryos were PGT-A tested and normal, why did my transfer still fail?”
That’s an important question. If the seed is healthy, it may be the soil—your uterus—that needs closer attention.
2. Uterine Factors (The “Soil”)
A healthy, receptive uterus is essential for successful implantation. Problems here can be structural, timing-related, or environmental.
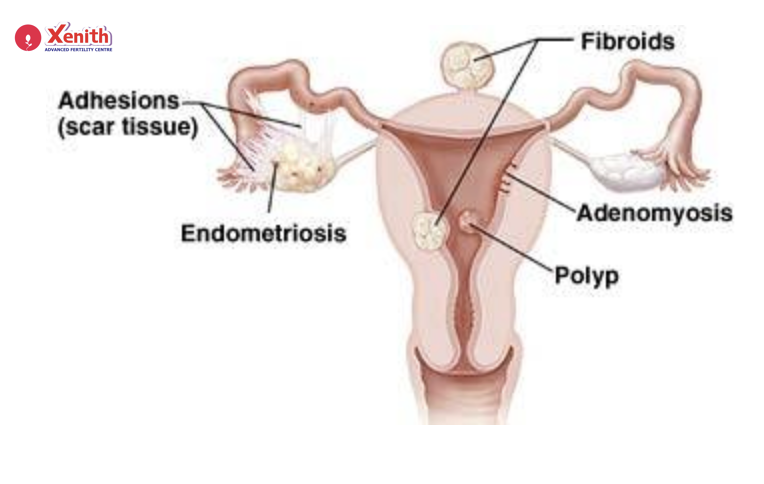
- Anatomical Issues:
Sometimes, the physical shape of the uterus prevents embryos from attaching properly.
Conditions like polyps, fibroids, scar tissue (adhesions), or a uterine septum can create a hostile surface for implantation.
Diagnosis: These are best detected through hysteroscopy (a camera-based inspection) or a 3D ultrasound
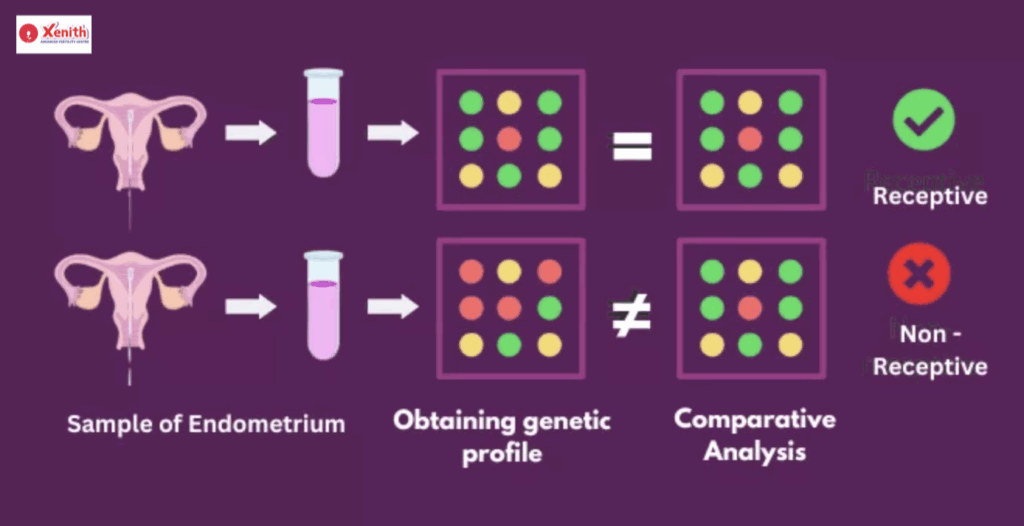
- Endometrial Receptivity (The “Timing”):
Even with a healthy uterus, timing matters. The uterus has a short, optimal window—called the Window of Implantation (WOI)—when it’s ready to accept an embryo.
For some women, this window is “displaced,” meaning the embryo is transferred too early or too late.
Diagnosis: The ERA (Endometrial Receptivity Analysis) test helps determine your unique WOI, allowing doctors to time the transfer precisely.
• Endometrial Environment (The “Health”):
The uterine lining can also be affected by subtle, hidden conditions.
- Chronic Endometritis (CE): A low-grade, often symptomless infection or inflammation that makes the lining unreceptive.
- Uterine Microbiome Imbalance: A healthy uterus should be rich in Lactobacillus bacteria, which support implantation.
Diagnosis:
- EMMA (Endometrial Microbiome Metagenomic Analysis) tests for microbiome balance.
ALICE (Analysis of Infectious Chronic Endometritis) detects harmful bacteria causing CE.
3. Systemic Factors (The “Whole Body”)
Sometimes, the problem isn’t in the uterus or embryo, but in how your body responds.
• Immunological Issues:
Your immune system’s job is to protect you—but occasionally, it becomes overprotective. Specialized immune cells like Natural Killer (NK) cells or other immune responses might mistakenly attack the embryo, treating it as a threat.
Diagnosis: An immunological RIF blood panel can detect such immune-related abnormalities.
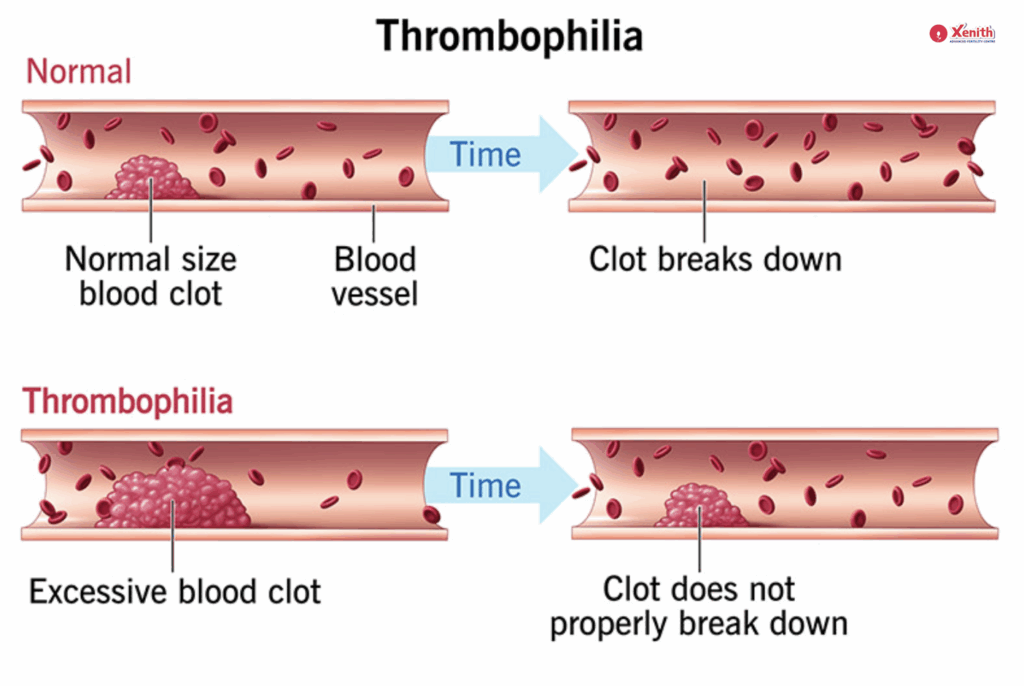
• Thrombophilia (Clotting Disorders):
Tiny, undetectable blood clots can obstruct blood flow to the implanting embryo.
Diagnosis: A thrombophilia panel checks for clotting disorders like Antiphospholipid Syndrome, which can hinder implantation and early pregnancy development.
Part 2: The “What Next” — Creating an Action Plan for RIF
When facing repeated IVF failures, it’s easy to feel lost in a maze of medical jargon. But the process doesn’t have to be random or confusing. A structured, step-by-step investigation can help uncover the missing pieces.
Step 1: A Thorough Review (What We Already Know)
Start with your history.
Your doctor will review previous IVF cycles—looking at embryo quality, transfer technique, and medication protocols. Sometimes, small changes here can make a big difference before you move on to more advanced testing.
Step 2: Investigate the Uterus (The “Soil”)
If you haven’t already, your fertility specialist may suggest a hysteroscopy, considered the “gold standard” for visually examining the uterine cavity. This allows direct identification and removal of abnormalities like fibroids or polyps.
Next, an endometrial biopsy may be performed. The same biopsy sample can often be used for three critical tests:
- ERA – checks implantation timing.
- EMMA – evaluates microbiome balance.
- ALICE – screens for chronic infection.
These tests together provide a comprehensive view of your uterine health and readiness.
Step 3: Investigate Systemic Factors (The “Body”)
Finally, your doctor may order a RIF blood panel, which includes immunological and thrombophilia tests. These help identify immune overactivity or clotting tendencies that may silently interfere with implantation.
Part 3: Advanced Treatment Strategies Based on Your Diagnosis
This is the section of hope—because once a cause is identified, there’s almost always a corresponding treatment.
If the issue is Anatomical:
- Treatment: Surgical correction through procedures like polypectomy or hysteroscopic removal of fibroids can restore a normal uterine cavity.
If the issue is Timing (Displaced WOI):
- Treatment: A Personalized Embryo Transfer (pFET), where the timing of progesterone administration is adjusted to match your unique receptivity window.
If the issue is the Environment (CE or Microbiome):
- Treatment: Antibiotics may be prescribed to treat infection, followed by vaginal or oral probiotics to rebuild a Lactobacillus-rich, healthy microbiome.
If the issue is Immunological or Clotting:
- Treatment: Your doctor may suggest blood thinners (like low-dose aspirin or Lovenox) or immune-modulating therapies (such as steroids or intralipids) to support implantation.
Conclusion: Moving from “Unexplained” to “Understood”
Recurrent Implantation Failure can feel like an endless series of “no’s.” But in reality, each failed cycle is an opportunity for answers. The goal is not to label your journey as “unexplained” but to uncover what’s been hidden all along.
With today’s advanced diagnostic tools and personalized treatments, RIF is rarely a dead end—it’s often a detour that leads to deeper understanding.
So, if you’re struggling with repeated IVF failures, don’t lose hope. This is your sign to ask for a deeper investigation. Schedule a consultation with Xenith Fertility Centre so we can create a personalized diagnostic and treatment plan for you.
FAQ
RIF is diagnosed after multiple failed IVF cycles despite transferring high-quality embryos—usually after 2–3 attempts.
There’s no single cause. It’s usually due to one or more factors:
1.Genetic issues in embryos.
2.Uterine abnormalities or timing problems.
3.Systemic immune or clotting disorders.
If the embryos are normal, the likely issue lies in the uterine lining’s health or timing, or in systemic immune reactions that prevent implantation.
A thorough RIF workup includes hysteroscopy, blood tests for immune and clotting issues, and an endometrial biopsy for ERA, EMMA, and ALICE testing.
Yes—absolutely. Identifying the specific cause allows for a targeted treatment plan. Many couples conceive successfully after addressing the underlying issue.