A diagnosis of zero sperm count (Azoospermia) is not the end of the journey. Learn about advanced sperm retrieval techniques like Micro-TESE available in Pune, and find out how you can still achieve biological fatherhood.
Introduction – Facing the Diagnosis
Understanding the “Zero Sperm Count” Diagnosis (Azoospermia)
Hearing the words “zero sperm count” can feel devastating. You may feel shocked, confused, angry, or even question your sense of masculinity. Many men describe this moment as one where the future they imagined suddenly feels uncertain. If you are going through this right now, know this first: you are not alone, and this diagnosis does not mean the end of your chance to become a biological father.
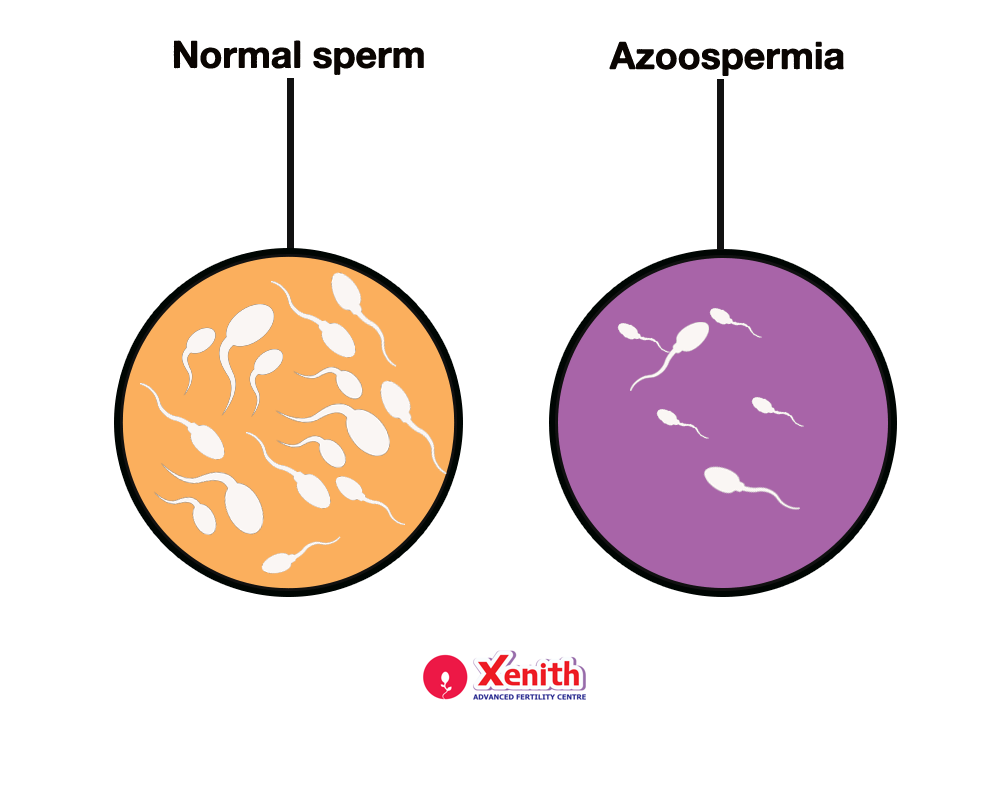
Medically, azoospermia means the complete absence of sperm in the ejaculate. It affects about 1% of all men and nearly 10–15% of men seeking fertility treatment. While the term sounds final, modern reproductive medicine has rewritten what “possible” looks like for men with this condition.
The Two Types: Obstructive vs. Non-Obstructive
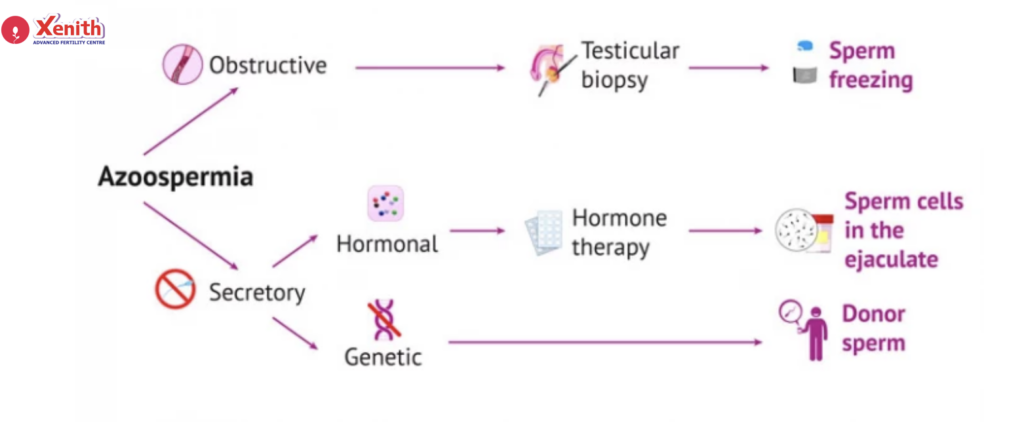
Azoospermia is not a single condition. It falls into two broad categories, and understanding which type you have is the key to your treatment plan.
- Obstructive Azoospermia (OA): Your body is producing sperm, but a blockage somewhere in the reproductive tract prevents sperm from reaching the semen.
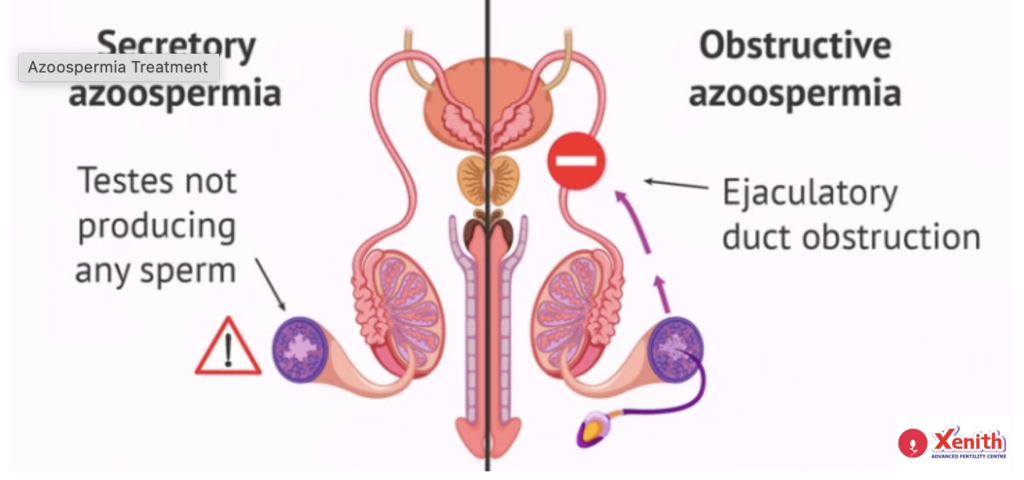
- Non-Obstructive Azoospermia (NOA): The issue lies in sperm production itself, which may be low, patchy, or severely impaired.
This distinction matters because it determines how sperm can be retrieved. The good news? Advanced techniques exist for both types, and this guide will walk you through them.
The Diagnostic Roadmap
Beyond a Simple Semen Analysis
A single semen analysis showing zero sperm is never the end of the investigation—it is just the beginning. To truly understand your condition, your doctor will guide you through a structured diagnostic roadmap.
You can expect:
- Repeat semen analysis to confirm the diagnosis.
- Hormone testing, especially FSH and testosterone, to understand how your testes are functioning.
- Genetic testing, such as karyotyping and Y-chromosome microdeletion analysis, to identify inherited causes that may affect sperm production and guide expectations.
These tests are not meant to overwhelm you—they are meant to ensure that no opportunity is missed.
Imaging: What an Ultrasound Can Tell Us
Imaging plays a crucial role, especially when obstruction is suspected. A scrotal ultrasound can evaluate testicular size, structure, and the presence of dilated ducts. A transrectal ultrasound (TRUS) can identify blockages in the ejaculatory ducts or seminal vesicles.
For many men, these scans provide clarity and, in some cases, immediate relief—because finding a blockage often means sperm retrieval is more straightforward.
Advanced Sperm Retrieval Techniques
The Gold Standard for Non-Obstructive Cases: Micro-TESE
If you have been told you have non-obstructive azoospermia, you may have already heard discouraging statements like “there is no sperm at all.” This is where Micro-TESE (Microdissection Testicular Sperm Extraction) changes everything.
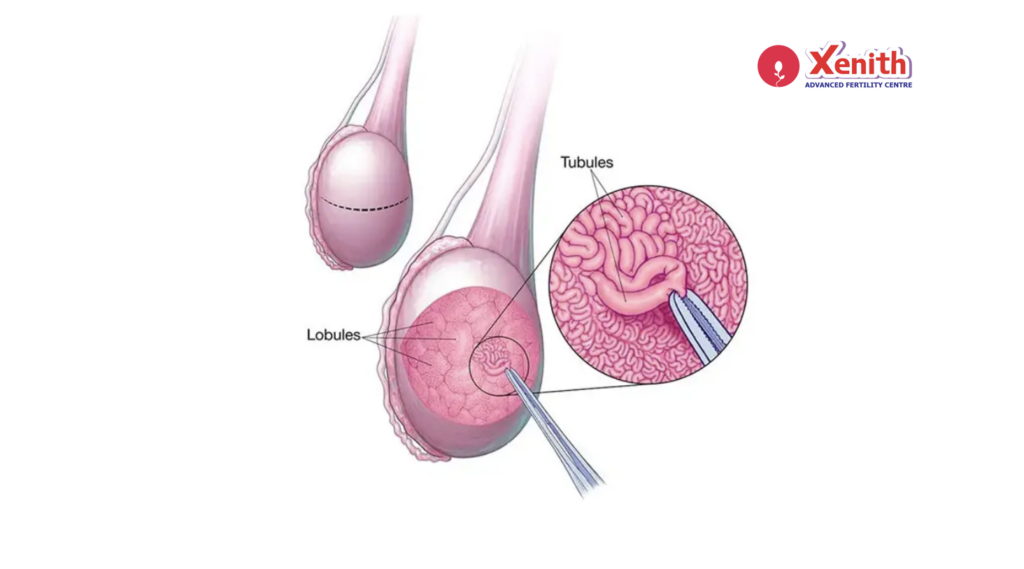
Micro-TESE is a highly advanced microsurgical procedure performed using a high-powered operating microscope. Instead of blindly removing testicular tissue, the surgeon carefully examines the testis to identify tiny pockets where sperm production may still be happening.
Why this matters to you:
- It offers higher sperm retrieval rates compared to conventional TESE.
- It causes less damage to testicular tissue.
- It provides hope even when previous biopsies or reports were negative.
For many men with NOA, Micro-TESE has been the turning point—the procedure that made biological fatherhood possible when all other doors seemed closed.
Options for Obstructive Azoospermia (PESA/MESA)
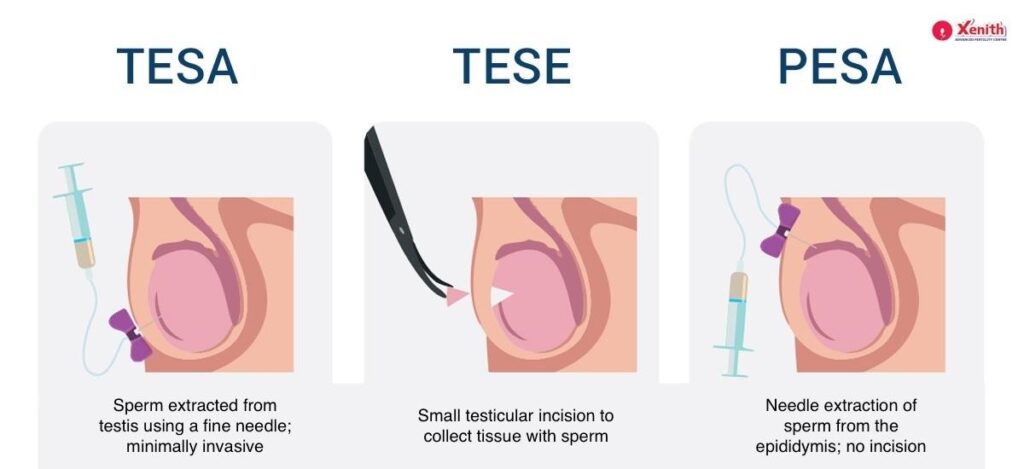
If your diagnosis is obstructive azoospermia, the approach is usually simpler and less invasive.
- PESA (Percutaneous Epididymal Sperm Aspiration): A needle-based technique to retrieve sperm directly from the epididymis.
- MESA (Microsurgical Epididymal Sperm Aspiration): A more precise microsurgical method that allows larger quantities of high-quality sperm to be retrieved.
Because sperm production is normal in these cases, retrieval success rates are typically very high. For you, this often means fewer procedures and excellent outcomes with assisted reproduction.
The Surgical Procedure & Recovery
Preparing for Micro-TESE
Preparation is straightforward. You may be advised to stop certain medications, avoid smoking or alcohol, and fast for a few hours before surgery. Most importantly, your care team will ensure you understand the procedure clearly—because confidence and calm matter.
What to Expect on the Day
Micro-TESE is performed under anesthesia, so you will not feel pain during the procedure. Using the microscope, the surgeon carefully explores the testicular tissue to locate areas likely to contain sperm. The procedure typically takes a few hours, depending on complexity.
You are not expected to “do” anything—your role that day is simply to rest and trust the expertise guiding you.
Post-Procedure Care and Next Steps
Recovery is usually smooth. Mild discomfort, swelling, or soreness is common and manageable with medication and brief rest. Most men return to normal activities within a few days.
Crucially, any sperm retrieved is immediately frozen (cryopreserved). This ensures it is safely stored and ready for use in an IVF cycle with ICSI, without the need to repeat surgery.
Your Specialized Solution in Pune
Why Expertise in Micro-TESE Matters
Micro-TESE is not a routine procedure. It requires:
- A trained microsurgeon with specific expertise in male infertility.
- A high-tech embryology lab capable of identifying and handling very few, fragile sperm.
- Seamless coordination between surgical and IVF teams.
This level of specialization is available only at select centers. At Xenith IVF, Pune, we focus on exactly these “difficult” cases—men who have been told elsewhere that nothing can be done.
Combining Retrieval with ICSI
Once sperm is retrieved, fertilization is achieved using ICSI (Intracytoplasmic Sperm Injection), where a single sperm is injected directly into an egg. This technique maximizes fertilization chances, even when sperm numbers are extremely low.
Conclusion
A Path to Fatherhood, Despite the Odds
Azoospermia is a serious diagnosis—but it is not a permanent barrier to fatherhood. Advances like Micro-TESE, PESA, MESA, and ICSI have transformed outcomes for men once considered untreatable.If you are facing zero sperm count today, remember this: your journey is not over. With the right expertise, technology, and individualized care, biological fatherhood is still within reach.
If you have been diagnosed with azoospermia, don’t give up hope. Schedule a confidential consultation with our male fertility specialist at Xenith IVF, Pune, to discuss your Micro-TESE options and your personalized path to fatherhood.