If you and your partner have been trying to conceive without success, you might be surprised to learn that low sperm motility is one of the most common reasons for male infertility. Simply put, sperm motility is the ability of sperm to swim forward efficiently—and when this movement is slow or uncoordinated, fertilization becomes more challenging.
The good news? Low sperm motility, or asthenozoospermia, is often manageable with the right diagnosis and treatment. Whether your goal is natural conception or exploring assisted reproductive techniques, understanding the condition is the first step toward a solution.

Free Thursday Consultation
Book Your AppointmentThink of sperm motility as the “engine power” that helps sperm travel through the female reproductive tract to meet and fertilize the egg. Without good motility, sperm may struggle to reach the egg at all.
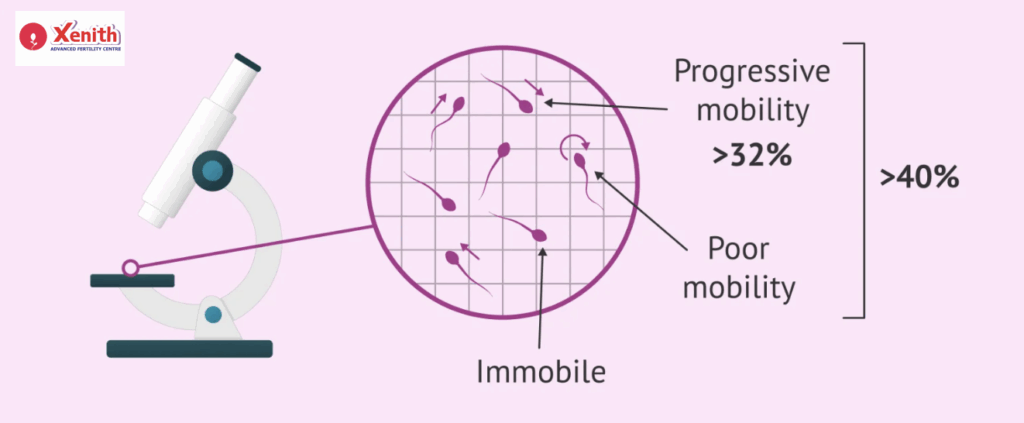
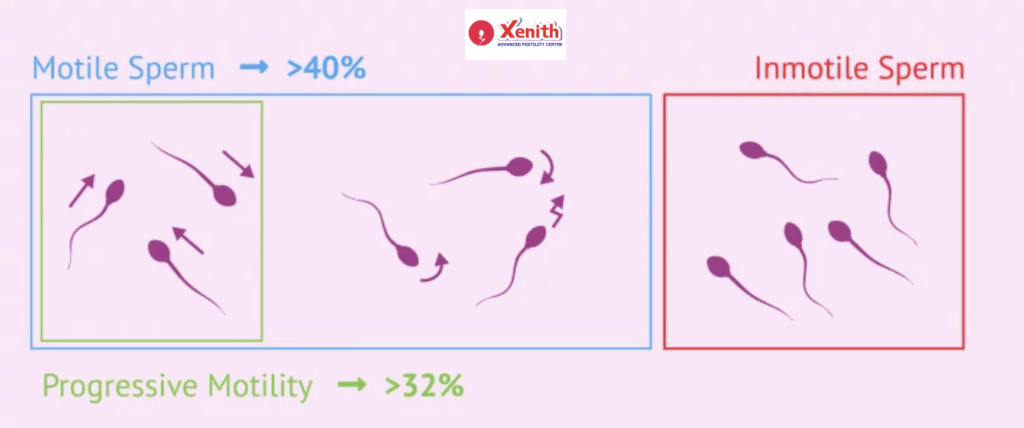
The World Health Organization (WHO) considers normal motility to be:
- Total motility (progressive + non-progressive): ≥ 40%
- Progressive motility (actively moving forward): ≥ 30%
Anything lower than these ranges can reduce the chances of natural conception.
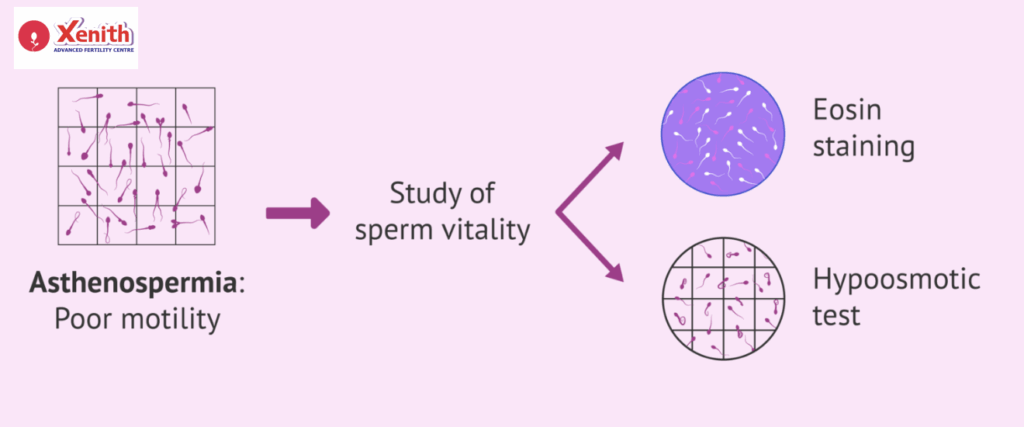
What Is Asthenozoospermia?
Asthenozoospermia is the medical term for low sperm motility. It’s measured in two ways:
- Total motility: The percentage of all moving sperm, even if they’re just twitching.
- Progressive motility: The percentage moving in a straight line or large circles toward the egg—this is the most important type.
Doctors classify it as:
- Mild: Slightly below WHO ranges
- Moderate: Noticeably reduced movement
- Severe: Very few or no sperm moving forward
Symptoms & When to Get Tested
Here’s the tricky part—you won’t notice physical symptoms of low motility. The main red flag? Difficulty conceiving despite regular, unprotected intercourse.
Experts recommend a semen analysis if:
- You’ve been trying for 6–12 months without success (shorter if your partner is over 35).
- You have risk factors like varicocele, hormonal problems, or past testicular injury.
Causes of Low Sperm Motility
Low motility can happen for many reasons, sometimes in combination:
- Varicocele – Enlarged veins in the scrotum that affect sperm quality.
- Hormonal imbalance – Low testosterone or other hormonal disruptions can impair sperm movement.
- Infections – Such as STIs or prostatitis, which can damage sperm.
- Lifestyle factors – Smoking, alcohol, heat exposure from saunas, hot baths, or laptops.
- Nutritional deficiencies – Low zinc, CoQ10, vitamin C, or omega-3 fatty acids.
- Genetic disorders – Rare but can impact sperm tail structure.
- Obesity & poor metabolic health – Linked to lower motility and sperm count.
- Environmental toxins or medications – Pesticides, radiation, chemotherapy, or certain drugs.
How Is Low Sperm Motility Diagnosed?
A semen analysis is the primary test. It evaluates:
- Sperm count
- Motility (progressive, non-progressive, immotile)
- Morphology (shape)
If needed, your doctor may also order:
- DNA fragmentation tests to check sperm health
- Scrotal ultrasound to detect varicocele or blockages
- Hormone testing for testosterone,FSH, LH, prolactin
Can You Get Pregnant with Low Sperm Motility?
Yes—especially if your case is mild. Many couples conceive naturally when other sperm parameters are healthy. In moderate to severe cases, medical intervention often improves the chances.
Your success also depends on:
- Overall sperm count
- Sperm shape (morphology)
- Female partner’s age and fertility status
Treatment Options for Low Sperm Motility
A. Lifestyle & Home Remedies
Small changes can make a big difference over time:
- Nutritional upgrades: Eat antioxidant-rich foods, add CoQ10, omega-3s, zinc, and vitamins C & E.
- Exercise & weight control: Improves testosterone and overall reproductive health.
- Reduce heat exposure: Avoid hot tubs, tight underwear, and prolonged laptop use on your lap.
- Quit smoking & limit alcohol: Both directly harm sperm motility.
B. Medical & Surgical Options
If an underlying cause is found, targeted treatment works best:
- Treat infections with antibiotics.
- Varicocele surgery to improve testicular blood flow.
- Hormonal therapy if testosterone or other hormone levels are low.
C. Assisted Reproductive Techniques (ART)
When lifestyle or medical treatments aren’t enough:
- IUI (Intrauterine Insemination) – Best for mild to moderate motility issues.
- IVF-ICSI – In severe cases, a single healthy sperm is injected directly into the egg.
- TESE (Testicular Sperm Extraction) – Retrieves sperm directly from the testicle if none are present in the semen.
Prognosis and Chances of Improvement
With consistent effort, sperm motility can improve—especially when the cause is lifestyle-related. Expect changes within 3–6 months, as that’s how long it takes to produce a new batch of sperm.
When to See a Fertility Specialist
Seek expert help if:
- You’ve tried for a year (or 6 months if your partner is over 35)
- Your semen analysis shows low motility
- You have known risk factors like varicocele or hormonal imbalance
At Xenith IVF, your first consultation includes a detailed semen evaluation, hormonal testing, and a personalized plan based on your fertility goals.
Why Choose Xenith IVF for Male Infertility Treatment?
When it comes to male infertility issues like low sperm motility, choosing the right clinic can make all the difference. At Xenith IVF, we combine medical expertise, advanced technology, and personalized care to maximize your chances of success.
- Expert Male Fertility Care – Our andrologists and reproductive specialists are experienced in diagnosing and treating even complex motility problems.
- Comprehensive Diagnostics – From detailed semen analysis to hormone testing and scrotal ultrasound, we thoroughly investigate the root causes.
- Tailored Treatment Plans – We address your unique situation, starting with lifestyle changes and supplements, moving to medical or surgical solutions, and using ART methods like IUI or IVF-ICSI when needed.
- Proven ICSI Success Rates – For severe motility cases, our ICSI expertise ensures even a single healthy sperm can lead to fertilization.
- Supportive, Confidential Environment – We understand the sensitivity of male infertility and offer compassionate guidance throughout your journey.
With Xenith IVF, you get more than treatment—you get a partner committed to helping you achieve your dream of parenthood.
Low sperm motility may feel discouraging, but it’s far from the end of your parenthood journey. With today’s medical advancements, most men with asthenozoospermia can become fathers—either naturally or with assistance. The key is early testing, accurate diagnosis, and targeted treatment.
Yes—depending on severity. ART methods like IUI or IVF-ICSI improve chances significantly.
Common causes include varicocele, infections, hormonal imbalance, poor lifestyle habits, and genetics.
Often yes, with diet, exercise, supplements, and avoiding heat and toxins.
It depends on the cause—options include lifestyle changes, medication, or ART like IVF-ICSI.
Typically 3–6 months after starting treatment or lifestyle changes.