If you’ve been trying to understand why fertility challenges persist despite healthy habits, you’re not alone. The connection between gut health and fertility can feel confusing, full of scientific jargon and conflicting wellness claims. You’ve probably seen countless supplements, “gut detoxes,” and hormone-balancing diets—but it’s hard to tell what’s actually backed by science.
This guide is here to change that. We’ll simplify the science behind the gut–fertility axis and help you understand how nurturing your gut can support both male and female reproductive health. By the end, you’ll have a clear, practical plan—no gimmicks, no guesswork.

Free Thursday Consultation
Book Your Appointment
The Science: What Is the Gut–Fertility Axis?
Your gut is home to trillions of microbes—bacteria, fungi, and other microorganisms—collectively known as the gut microbiome. These tiny residents play a big role in digestion, immunity, metabolism, and yes, reproductive health.
When your gut bacteria are balanced, your body functions smoothly. But when this balance is disrupted—a state called gut dysbiosis—it can trigger inflammation, alter hormone levels, and disturb your body’s natural rhythms.
The Gut–Hormone Connection
Your gut doesn’t just digest food; it communicates with your endocrine system (the body’s hormone regulator). Through this gut–hormone axis, it influences the production and metabolism of hormones like estrogen, testosterone, and insulin—all vital for fertility.
The Estrobolome

Within your gut microbiome lies a specialized group of bacteria called the estrobolome. These microbes help metabolize and balance estrogen, ensuring that your levels stay optimal. When the estrobolome is out of balance, estrogen can either build up or be flushed out too quickly—both scenarios that can interfere with ovulation, implantation, and sperm production.
Understanding these basics sets the stage for seeing just how deeply your gut impacts fertility—for both women and men.
How Gut Health Specifically Affects Female Fertility
The Inflammation Link: “Leaky Gut” and Ovulation
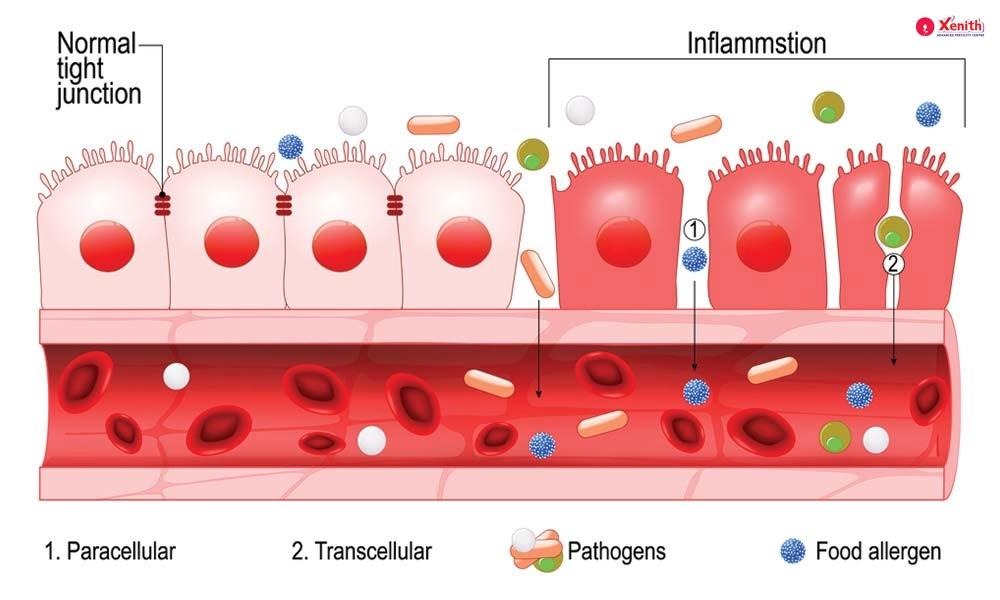
A “leaky gut” happens when the gut lining becomes compromised, allowing toxins and inflammatory molecules to enter the bloodstream. This triggers systemic inflammation, which can disrupt the hormonal signals necessary for ovulation. Chronic inflammation can also affect the quality of eggs and the receptivity of the uterine lining, making conception harder.
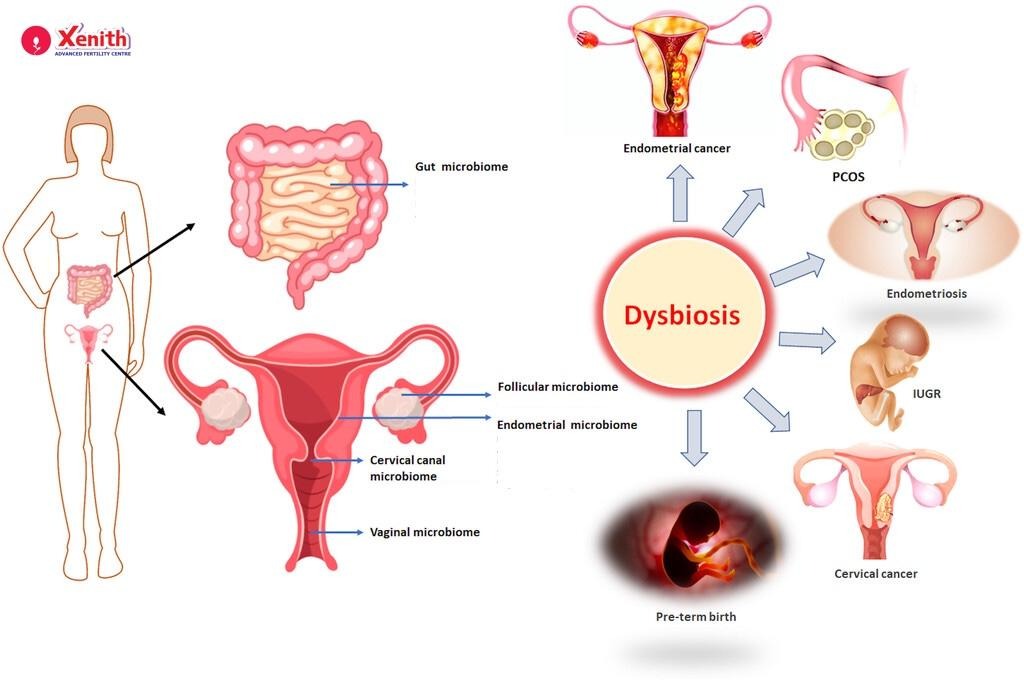
Gut Dysbiosis and Fertility Conditions: PCOS & Endometriosis
Two of the most common fertility challenges—PCOS (Polycystic Ovary Syndrome) and endometriosis—have deep links to gut imbalance.
- In PCOS, dysbiosis contributes to insulin resistance and low-grade inflammation, both of which disrupt ovulation.
- In endometriosis, researchers have found altered gut microbiota that promote inflammation and estrogen dominance—conditions that worsen pain and reduce fertility.
By addressing gut imbalance, you’re not just helping your digestion—you’re targeting some of the root causes of these complex conditions.
The Vaginal Microbiome: Your Gut’s Critical Neighbor
Few people know that the vaginal microbiome is closely connected to gut health. In fact, beneficial bacteria from your gut (especially Lactobacillus species) help seed and maintain a healthy vaginal environment.
A Lactobacillus-dominant vaginal microbiome supports fertility by:
- Lowering vaginal pH to prevent infections
- Promoting healthy cervical mucus
- Creating an optimal environment for embryo implantation
This is particularly crucial for women undergoing IVF or fertility treatments, where even small imbalances in vaginal flora can influence success rates.
The Missing Piece: Why Gut Health Matters for Male Fertility
When it comes to fertility, men are half the equation—but gut health for male fertility is rarely discussed.
Introducing the “Gut–Testis Axis”
Emerging research reveals a powerful link between gut health and sperm quality, known as the gut–testis axis. Inflammation or dysbiosis in the gut can lead to oxidative stress and hormonal imbalance, reducing sperm count, motility, and morphology.
Moreover, an imbalanced gut can lower testosterone levels, affecting libido and sperm production. Supporting gut health, therefore, can help improve overall male reproductive potential—making it an essential focus for couples trying to conceive.
A 5-Step Practical Plan to Improve Gut Health for Fertility
It’s time to turn insight into action. Here’s your practical, science-backed plan to start improving gut health and fertility.
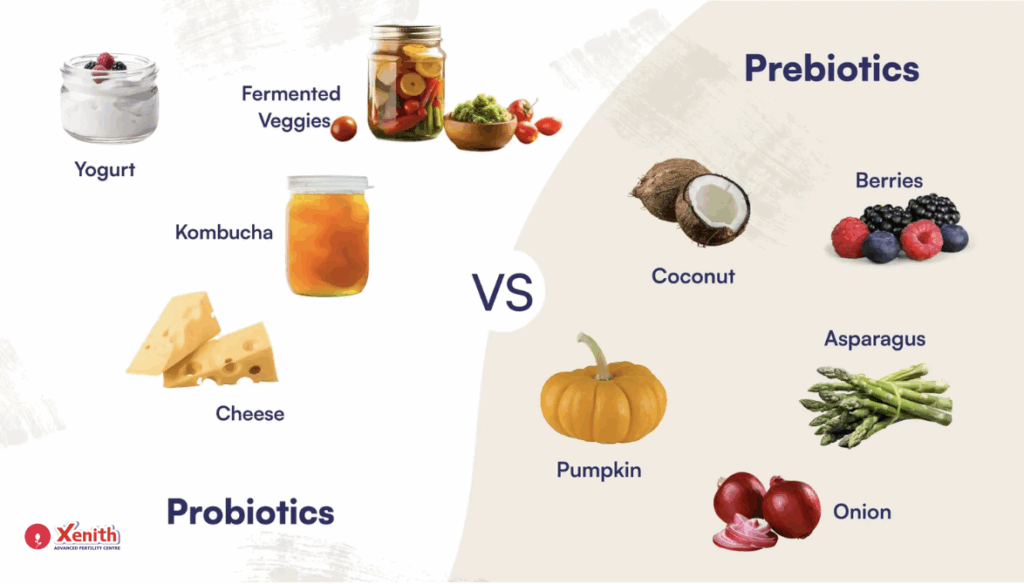
1. Eat for Your Microbes: The Prebiotic & Probiotic Diet
- Prebiotic Foods (feed good bacteria): Garlic, onions, asparagus, leeks, bananas, oats, flaxseeds.
- Probiotic Foods (add good bacteria): Yogurt, kefir, kimchi, sauerkraut, miso, and tempeh.
- Foods to Limit: Processed sugar, refined flour, alcohol, and artificial sweeteners—all of which disrupt microbial balance.
Try to include a variety of these foods daily. Think of your gut as a garden: prebiotics are the fertilizer, and probiotics are the seeds.
2. Smart Supplementation: Choosing the Right Probiotics
Not all probiotics are created equal. Choose research-backed strains that support reproductive and vaginal health:
- For women: Lactobacillus rhamnosus, Lactobacillus reuteri, Lactobacillus crispatus
- For men: Bifidobacterium longum and Lactobacillus plantarum (linked with better testosterone and sperm motility)
Always consult your healthcare provider before starting supplements—especially if you’re already taking fertility medication.
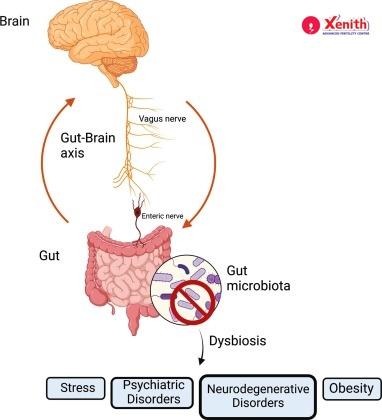
3. Manage the Gut–Brain Axis: Stress and Your Gut
Chronic stress damages the gut lining and changes microbiome diversity. Lowering stress helps restore gut balance and hormone regulation.
Try:
- Mindfulness or meditation (10 minutes daily)
- Light physical activity (like yoga or walking)
- Consistent sleep routine (7–8 hours)
- Breathwork or journaling before bed

Your mind and gut are constantly communicating—calming one helps the other.
4. Move Your Body (Gently)
Exercise improves digestion, reduces inflammation, and enhances mood. But there’s a catch: over-exercising can increase cortisol, the stress hormone that harms both gut and reproductive health.
Aim for moderate, regular movement—brisk walks, yoga, swimming, or cycling. Listen to your body instead of pushing it.
5. How to Test: When to Go Beyond Diet
If you’ve been consistent with dietary and lifestyle changes but still experience digestive issues, irregular cycles, or infertility, consider working with a qualified practitioner.
They may recommend:
- Comprehensive stool tests (to assess bacterial balance and inflammation)
- Hormone panels (to see how gut health affects your endocrine system)
These tests help identify deeper imbalances that diet alone can’t fix.
Conclusion: Your Gut Is a Foundation
Your gut isn’t just about digestion—it’s a control center for your entire body, influencing hormones, inflammation, and fertility. When you take care of it, you’re not chasing another health trend; you’re investing in the foundation of your reproductive and overall well-being.
So start simple. Add more fiber, manage your stress, move daily, and listen to your body. Over time, these small, consistent choices can make a big difference.
FAQ
Gut dysbiosis, leaky gut, and chronic inflammation can disrupt hormones, trigger autoimmune responses, and reduce nutrient absorption—all of which can make conception more difficult.
Yes. Certain Lactobacillus strains improve vaginal and uterine health, reduce inflammation, and create a more hospitable environment for conception and implantation.
Absolutely. When your gut lining leaks inflammatory molecules into your bloodstream, it can interfere with estrogen and insulin regulation—two hormones vital for fertility.
Through the gut–testis axis, poor gut health can reduce sperm quality, motility, and testosterone production—directly impacting fertility outcomes.
While it’s not a cure-all, improving gut health can address underlying issues like inflammation, hormone imbalance, and nutrient deficiency that often stand in the way of conception.