If you are reading this, it likely means you or someone you love has faced the heartbreak of losing a pregnancy more than once. Please know this: your pain is real, your grief is valid, and you are not alone. Recurrent pregnancy loss (RPL) is an emotionally heavy journey, and it is natural to feel confusion, sadness, or even guilt. But this is not your fault. There is hope, and there are answers.
Recurrent Pregnancy Loss is defined as the loss of two or more consecutive pregnancies. While this can feel overwhelming, medical science has advanced tremendously, and many people diagnosed with RPL eventually go on to have healthy pregnancies. This article will walk you through the possible causes, the diagnostic process, treatment options, and—most importantly—the hope that lies ahead. Our goal is to bring clarity, explain the science in simple terms, and light your path forward.

Free Thursday Consultation
Book Your Appointment- Why Does Recurrent Pregnancy Loss Happen? Exploring the Causes
- Genetic and Chromosomal Factors
- Uterine and Anatomical Issues
- Immunological and Autoimmune Factors
- Hormonal and Endocrine Imbalances
- Lifestyle and Environmental Factors
- Unexplained RPL
- Finding Answers: The Diagnostic Process for RPL
- Treatment and Next Steps: Your Path to a Healthy Pregnancy
- Moving Forward with Confidence at Xenith IVF
- Frequently Asked Questions (FAQ)
Why Does Recurrent Pregnancy Loss Happen? Exploring the Causes
In many cases, doctors can identify a specific cause for RPL—and often, it is something that can be treated. Understanding the “why” is the first step toward healing and planning the next chapter of your journey.
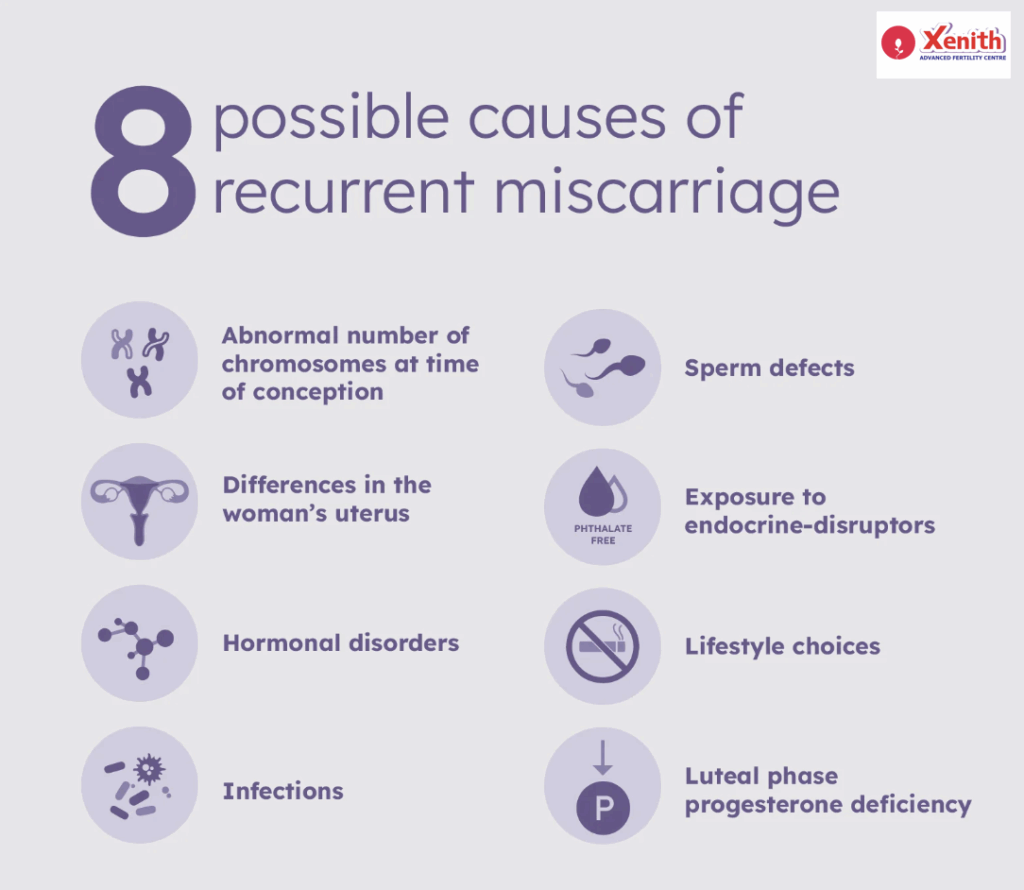
Genetic and Chromosomal Factors
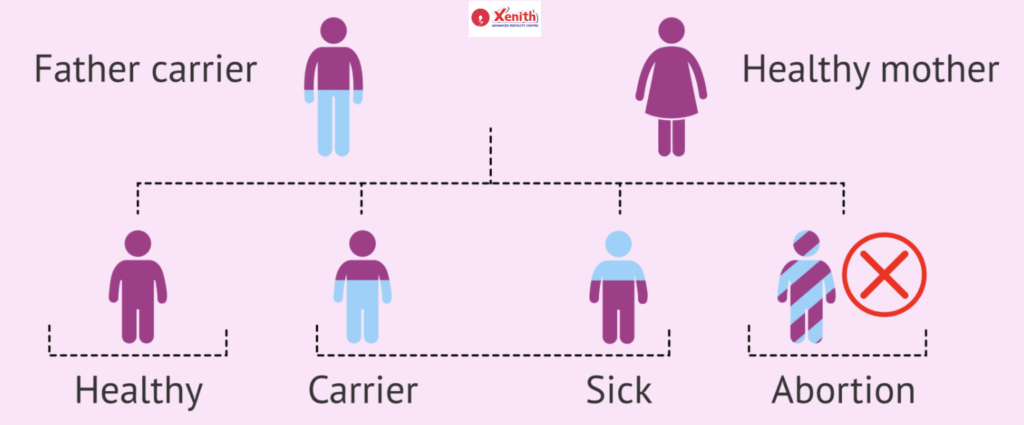
This is the most common reason behind recurrent miscarriages. Many pregnancy losses occur due to chromosomal abnormalities (called aneuploidy), where the embryo has too many or too few chromosomes. These changes usually happen by chance, but the risk does increase with maternal age.Sometimes, one parent may carry a condition called a balanced translocation, where their chromosomes are rearranged. While the parent remains healthy, this can cause embryos to develop with missing or extra genetic material, leading to miscarriage.
Uterine and Anatomical Issues
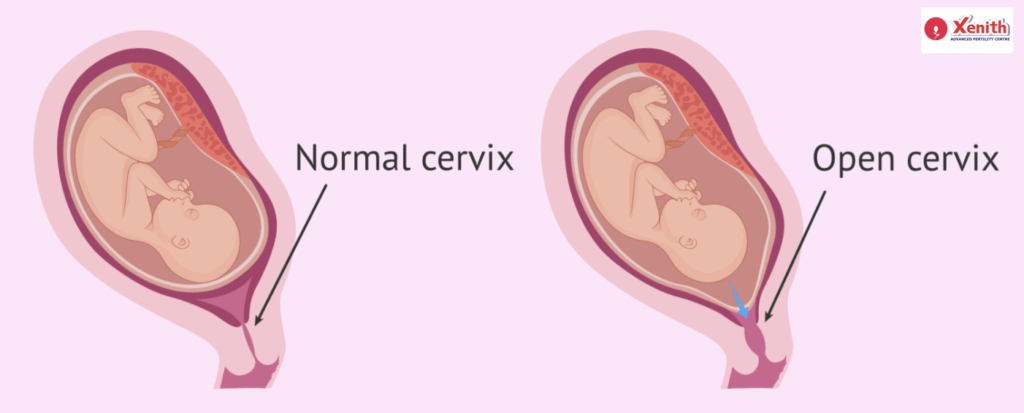
The uterus plays a vital role in supporting a pregnancy. Certain structural differences can interfere with implantation or fetal growth:
- Congenital conditions like a septate uterus (where a wall divides the uterine cavity).
- Acquired conditions such as fibroids, polyps, or adhesions. These may limit space in the uterus or reduce blood flow to the pregnancy.
Immunological and Autoimmune Factors
Our immune system is designed to protect us, but sometimes it mistakenly interferes with pregnancy. One well-known condition is Antiphospholipid Syndrome (APS), where abnormal blood clotting increases the risk of miscarriage. Other immune-related imbalances are being studied, and while they are less common, they may also contribute to RPL.
Hormonal and Endocrine Imbalances
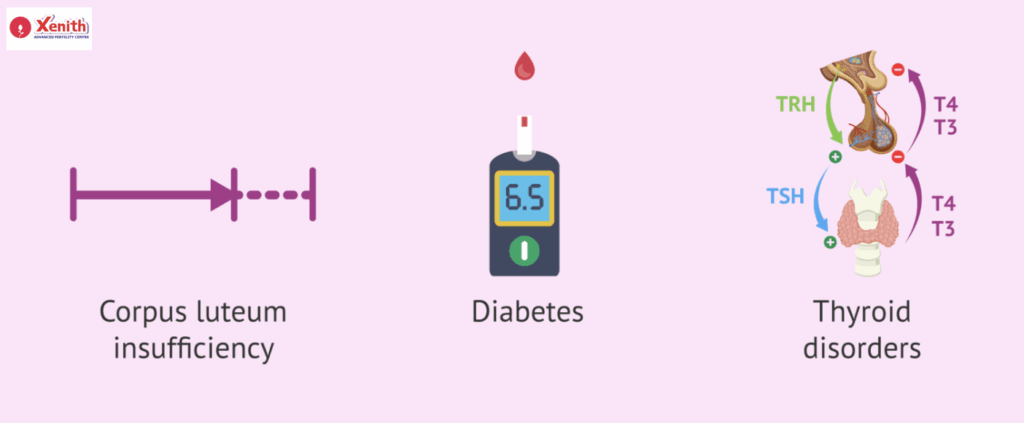
Hormones play a central role in establishing and maintaining pregnancy. Issues such as:
- Thyroid disorders (overactive or underactive thyroid).
- Diabetes that is not well-controlled.
- Low progesterone levels, which are essential for supporting early pregnancy.
Each of these can increase the risk of miscarriage but can often be managed with proper treatment.
Lifestyle and Environmental Factors
Sometimes, small changes in lifestyle can make a significant difference. Smoking, excessive alcohol use, obesity, or being severely underweight can affect both egg quality and uterine health. Environmental exposures, stress, and poor sleep can also play a role.
Unexplained RPL
For about 30–50% of couples, no specific cause is found. While this can feel frustrating, it is important to remember that many people with unexplained RPL still go on to have successful pregnancies with supportive care. The absence of an answer does not mean the absence of hope.
Finding Answers: The Diagnostic Process for RPL
Taking proactive steps toward answers can bring a sense of control during a difficult time. A thorough diagnostic process helps doctors tailor treatment to your unique situation.
The first step is a detailed medical history and consultation with a fertility specialist. This discussion covers previous pregnancies, medical conditions, lifestyle factors, and family history.
The RPL Test Panel may include:
- Karyotyping for both partners to detect chromosomal issues.
- Uterine evaluation, which may involve 3D ultrasound or hysteroscopy (a small camera inserted into the uterus).
This comprehensive approach ensures that nothing is overlooked, and every potential factor is addressed.
Treatment and Next Steps: Your Path to a Healthy Pregnancy
While the journey through RPL can feel isolating, medical solutions and supportive care offer real hope. Treatment focuses on addressing the root cause whenever possible.
Treating the Underlying Cause
- Surgical correction can fix uterine abnormalities like a septum, fibroids, or adhesions.
- Medical management is available for hormonal imbalances (e.g., thyroid medication, progesterone supplementation) and autoimmune conditions (e.g., blood thinners for APS).
- Lifestyle modifications such as quitting smoking, reaching a healthy weight, and managing stress can also improve outcomes.
Advanced Reproductive Technologies (ART)
When genetic factors are the main concern, In Vitro Fertilization (IVF) with Preimplantation Genetic Testing for Aneuploidy (PGT-A) is a powerful option. With this approach, embryos are created in a lab, tested for chromosomal health, and only chromosomally normal embryos are transferred into the uterus. This significantly reduces the chance of miscarriage due to genetic abnormalities.
Emotional Support and Counseling
The emotional toll of recurrent pregnancy loss is immense. Counseling, support groups, or therapy can provide a safe space to process grief and rebuild hope. Emotional well-being is not just supportive—it is an integral part of the healing journey.
Moving Forward with Confidence at Xenith IVF
A diagnosis of recurrent pregnancy loss does not mean you cannot build your family. With the right diagnosis, tailored treatment, and compassionate support, the chances of success are high.
At Xenith IVF, we understand that your journey is unique. Our team combines advanced science with heartfelt care, ensuring that you never walk this path alone. With us, hope is not just a word—it is a plan.
Your journey is unique, and you don’t have to walk it alone. If you’ve experienced multiple pregnancy losses, our compassionate team is here to provide answers and support. Contact Xenith IVF to schedule a comprehensive evaluation.

Frequently Asked Questions (FAQ)
The most common cause is genetic, where the embryo has an abnormal number of chromosomes. This usually happens by chance and becomes more likely with maternal age.
A comprehensive panel includes blood tests for hormonal and autoimmune disorders (like APS), genetic testing (karyotyping) for both partners, and imaging tests such as a 3D ultrasound or hysteroscopy to evaluate the uterus.
Absolutely. Even when no clear cause is found, the prognosis is often very good. With supportive care and, in some cases, treatments like IVF, many couples go on to have healthy babies.