When couples embark on the journey of IVF (in vitro fertilization), they often hope that science can bridge the gap where nature has created challenges. But for individuals living with autoimmune diseases, the path to parenthood can feel even more complicated. Autoimmune conditions don’t just affect daily health—they can also influence fertility and IVF outcomes. Understanding this connection is key to creating realistic expectations, adopting the right strategies, and most importantly, holding onto hope.
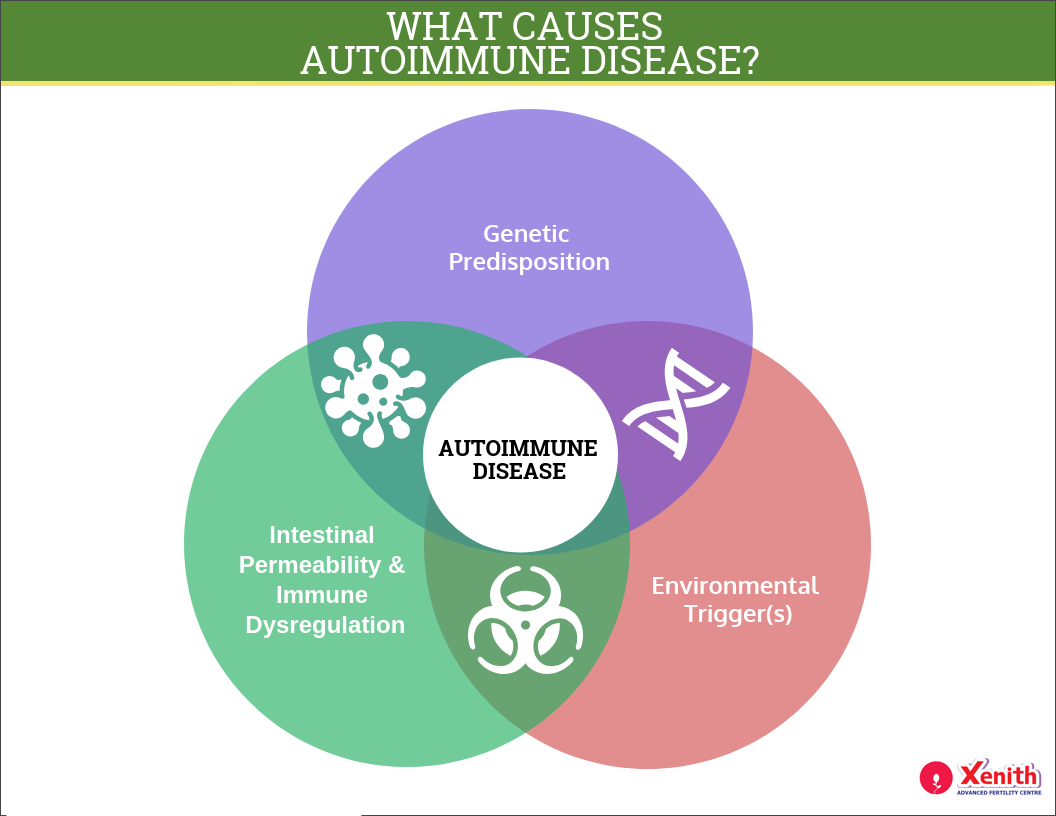
What are Autoimmune Diseases?
Autoimmune diseases occur when the immune system, which normally protects us from infections, mistakenly attacks our own cells and tissues. Instead of recognizing “self” from “foreign,” the immune system becomes confused and overactive. This self-directed attack can cause inflammation, tissue damage, and disruptions in how organs function.

Free Thursday Consultation
Book Your AppointmentThere are over 80 types of autoimmune diseases, but some commonly linked with fertility challenges include:
- Rheumatoid Arthritis (RA): A condition that causes joint inflammation but can also increase systemic inflammation in the body.
- Lupus (Systemic Lupus Erythematosus or SLE): A complex disease that can affect multiple organs, including the reproductive system.
- Hashimoto’s Thyroiditis: An autoimmune thyroid condition that can disrupt hormone levels essential for ovulation and pregnancy.
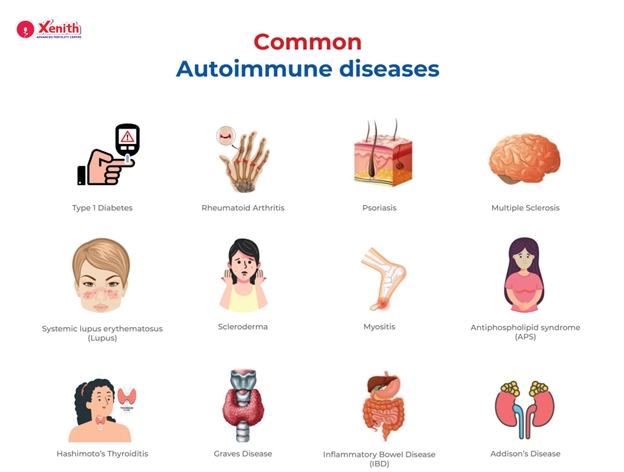
These conditions are more common in women of reproductive age, making their connection with fertility an important concern.
How Autoimmune Diseases Can Affect Fertility
Autoimmune diseases can influence fertility in several ways, depending on the condition and its severity. Some of the key mechanisms include:
- Hormonal Disruption: Autoimmune thyroid disorders, such as Hashimoto’s, can interfere with ovulation and menstrual regularity.
- Egg Quality and Ovarian Function: Chronic inflammation can damage ovarian tissue and impact egg health.
- Implantation Challenges: In some women, the immune system mistakenly attacks the embryo or the uterine lining, reducing the chances of implantation.
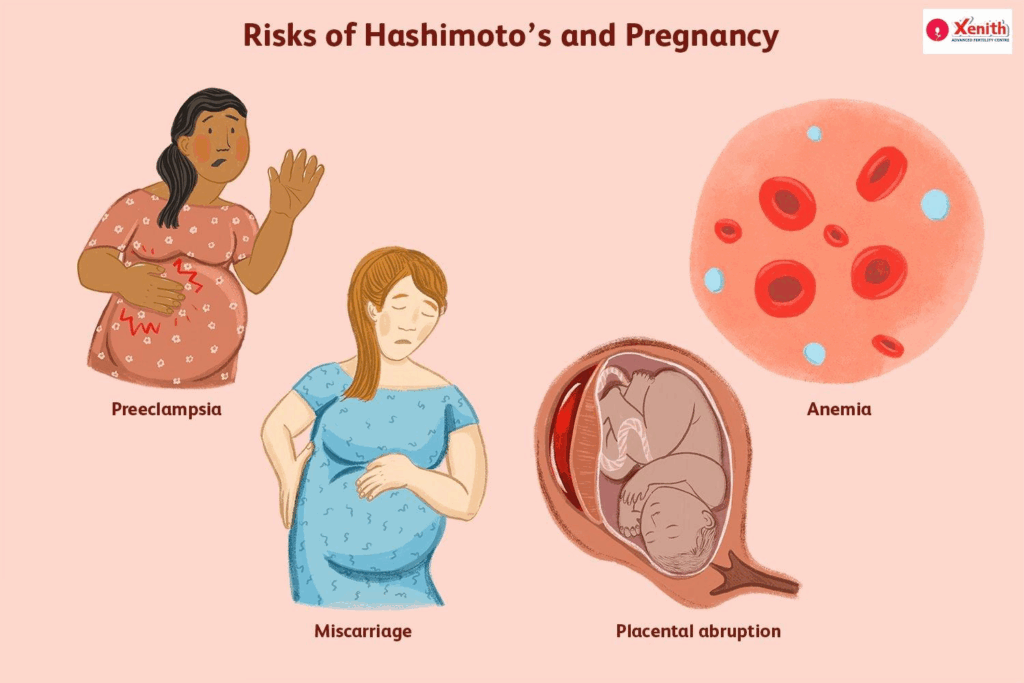
- Pregnancy Maintenance: Autoimmune activity may increase the risk of miscarriage due to clotting disorders, inflammation, or immune rejection of the fetus.
In short, while not every autoimmune patient experiences infertility, the immune system’s imbalance can create hurdles at multiple stages of conception and pregnancy.
The Impact of Autoimmune Diseases on IVF Success
IVF offers hope to many individuals with autoimmune diseases, but research shows that these conditions can affect treatment outcomes. For example:
- Women with lupus or antiphospholipid syndrome (APS) may have higher risks of miscarriage even after successful embryo transfer.
- Thyroid autoantibodies have been associated with lower fertilization and implantation rates.
- Chronic inflammation from autoimmune conditions can reduce egg quality, making it harder to create healthy embryos.
Challenges specific to IVF include:
- Poor Ovarian Response: Women with certain autoimmune conditions may produce fewer eggs during stimulation.
- Higher Implantation Failure Rates: The immune system may create an environment that is less welcoming for the embryo.
- Increased Pregnancy Complications: Even when IVF is successful, autoimmune activity may lead to complications such as preeclampsia or preterm birth.
Still, it’s important to note that many women with autoimmune diseases do have successful IVF pregnancies with proper management. The key lies in careful planning and support.
Strategies for Improving IVF Success in Patients with Autoimmune Diseases
Fortunately, there are multiple strategies to improve outcomes for patients undergoing IVF while managing autoimmune conditions:
1. Medical Management
- Immunosuppressants and Steroids: Carefully prescribed medications can reduce immune overactivity and improve embryo acceptance.
- Blood Thinners (e.g., heparin, aspirin): Used in conditions like APS to reduce the risk of clotting and miscarriage.
- Thyroid Hormone Replacement: Helps stabilize hormone levels in thyroid-related autoimmune conditions.
2. Lifestyle and Dietary Approaches
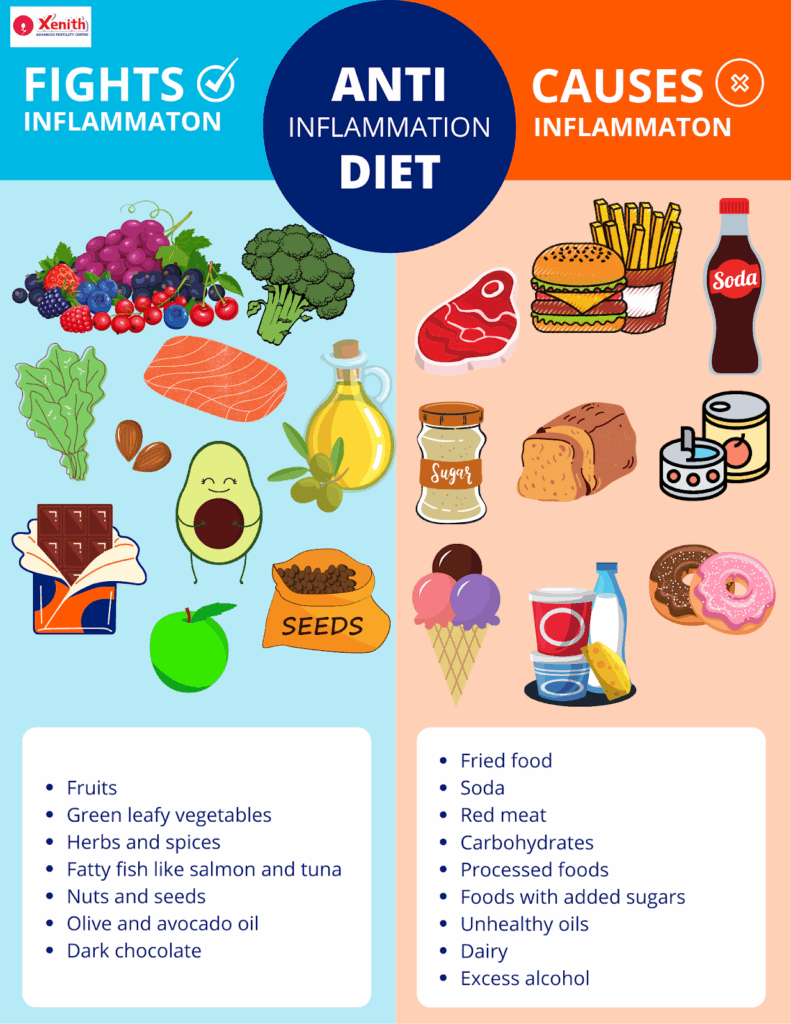
- Anti-inflammatory Diet: Emphasizing whole foods, leafy greens, omega-3 rich foods (flaxseeds, walnuts, fatty fish), and minimizing processed foods may reduce systemic inflammation.
- Stress Reduction: Stress can worsen autoimmune flare-ups. Practices like yoga, meditation, and gentle exercise may help.
- Adequate Sleep and Hydration: Both are vital for immune balance and overall fertility health.
3. Alternative and Complementary Therapies
- Acupuncture: Some studies suggest it may improve blood flow to the uterus and reduce stress.
- Mind-body Programs: Counseling and fertility support groups can provide emotional resilience during treatment.
When to Seek Expert Advice
If you have an autoimmune disease and are considering IVF, involving the right specialists is crucial.
- Fertility Specialists: They can design a personalized IVF protocol considering your medical background.
- Rheumatologists or Immunologists: They ensure your autoimmune condition is stable and managed before and during IVF.
- Endocrinologists: Especially for thyroid-related autoimmune conditions, hormone monitoring is essential.
Specialized testing, such as thyroid antibody tests, antiphospholipid antibody screening, or natural killer cell activity tests, can provide valuable insights into how autoimmune activity might affect your fertility journey.
Conclusion
The relationship between autoimmune diseases and IVF success is complex but not insurmountable. While these conditions can pose challenges in conception, implantation, and pregnancy maintenance, proactive management, medical interventions, and lifestyle adjustments can significantly improve outcomes.
For anyone navigating both autoimmune disease and infertility, it’s important to remember: you are not alone. Many individuals have successfully built families despite these challenges. With the right care team and strategies, there is real hope on this journey.
FAQ
Yes. Autoimmune diseases can affect fertility both directly (through ovarian damage, hormone disruption, or uterine inflammation) and indirectly (through overall health challenges or medication side effects).
The strongest links are with lupus, rheumatoid arthritis, Hashimoto’s thyroiditis, celiac disease, and antiphospholipid syndrome. These conditions can interfere with ovulation, implantation, or pregnancy maintenance.
They may lower egg quality, reduce fertilization rates, and increase the chances of implantation failure or miscarriage. Some conditions also heighten the risks of complications during pregnancy.
Yes. Tests may include thyroid antibody screening, ANA (antinuclear antibodies), antiphospholipid antibody panel, and specialized immune function tests. These help doctors identify risks and plan treatments.
Depending on the condition, doctors may prescribe steroids, immunosuppressants, thyroid hormone replacement, blood thinners, or low-dose aspirin. These medications must be carefully balanced to ensure both maternal health and embryo safety.
Yes. Anti-inflammatory diets, regular gentle exercise, stress-reduction practices, and proper sleep can support immune balance and improve the chances of IVF success. While lifestyle alone may not cure autoimmune issues, it plays a powerful supportive role.