If you’ve recently been diagnosed with an inguinal hernia or are recovering from hernia surgery, it’s natural to wonder whether this condition could affect your fertility. Many men worry that a bulge in the groin or any operation near the testicles might reduce sperm count or cause long-term reproductive problems.
The truth is more nuanced—and often more reassuring. While most inguinal hernias don’t cause infertility, certain situations can influence testicular health and sperm function. Understanding how hernias develop, what risks they pose, and when treatment can help is the first step toward protecting your reproductive future.

Free Thursday Consultation
Book Your AppointmentWhat Is an Inguinal Hernia and Why Can It Affect Fertility?
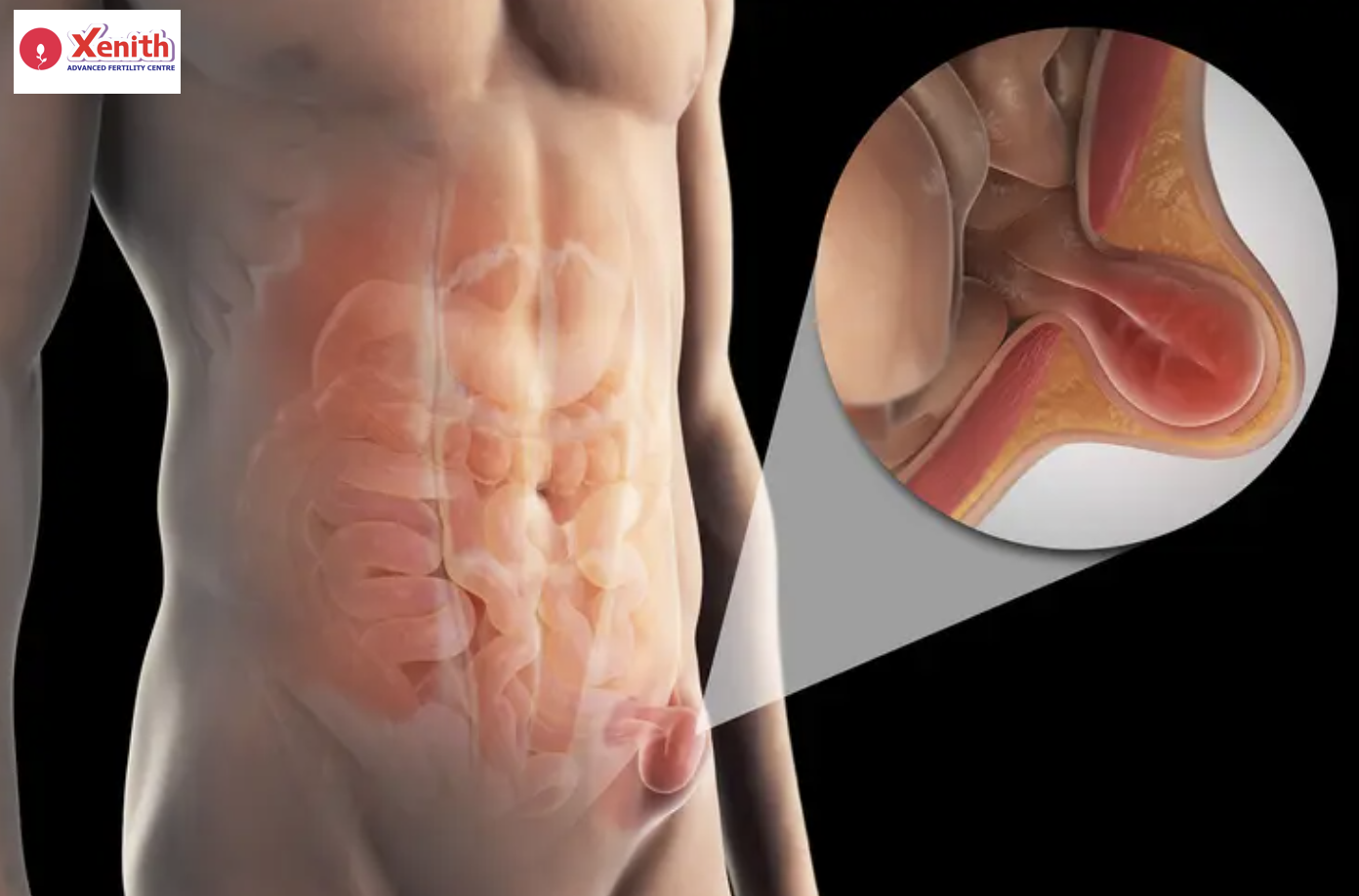
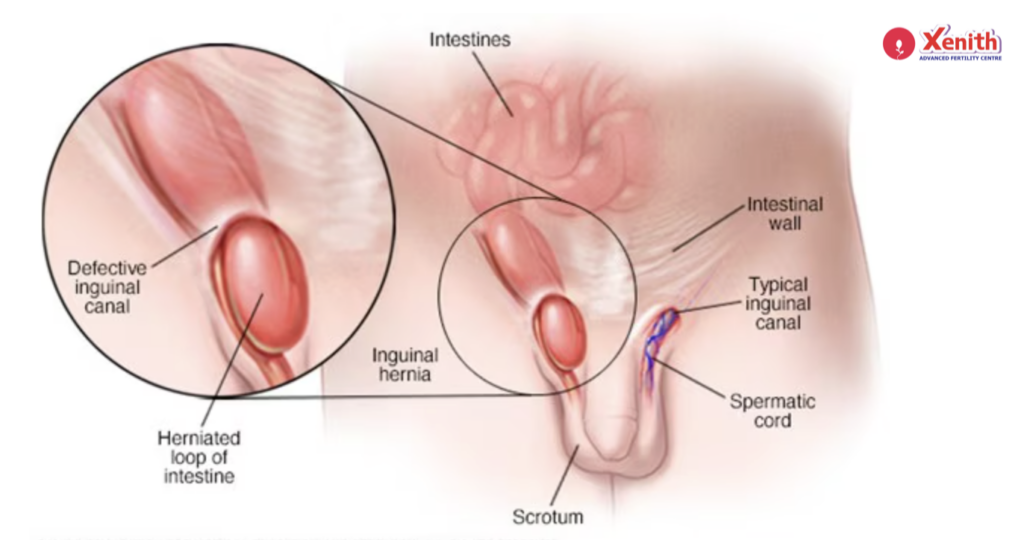
An inguinal hernia occurs when abdominal tissue—usually intestine or fat—pushes through a weak spot in the lower abdominal wall, creating a bulge in the groin. This is the most common type of hernia in men because the inguinal canal is where the testicles descend before birth, leaving behind a potential weak point.
You might wonder why this matters for reproductive health. The inguinal canal also carries the spermatic cord, which includes the vas deferens (the tube that transports sperm), blood vessels supplying the testicle, and nerves. Anything that increases pressure or disrupts these structures has the potential to influence fertility.
How Inguinal Hernias Develop
Understanding how hernias form can help you see why they may sometimes affect male fertility.
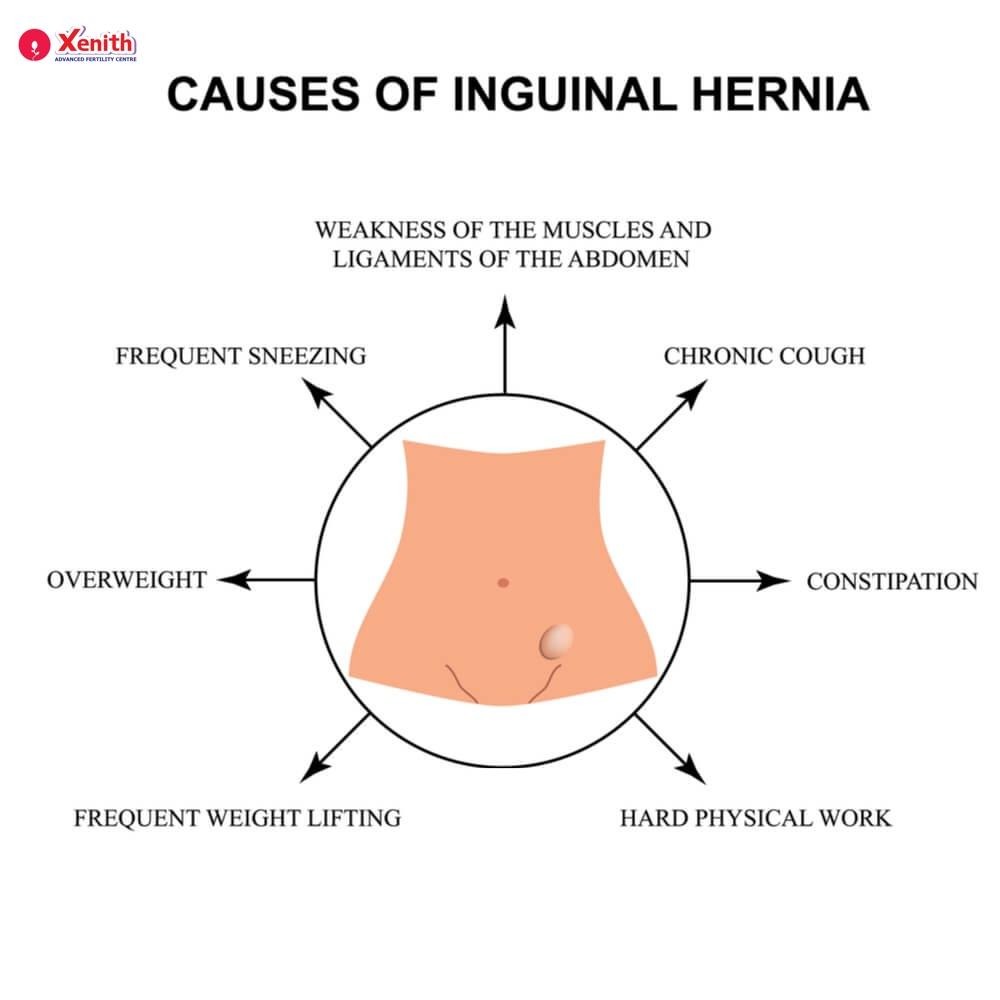
Common causes include:
- Congenital (present from birth) weakness in the abdominal wall
- Heavy lifting or straining
- Chronic coughing
- Obesity
- Previous surgeries in the groin
- Aging and muscle weakening
When tissue pushes through the canal, it can press on or stretch the spermatic cord. In most men, this pressure is mild and causes only discomfort or swelling. But in some cases, it can impact blood flow or temperature regulation—two key factors for sperm production.
Potential Ways Hernias Can Affect Fertility
Not every hernia affects fertility, but certain mechanical and physiological changes may influence sperm production or transport. Here’s what you need to know.
1. Pressure on the Spermatic Cord
The spermatic cord contains:
- Vas deferens (the sperm-transport tube)
- Testicular artery and veins
- Lymphatic vessels
- Nerves
A large or long-standing hernia may press on these structures, temporarily affecting sperm movement or testicular function.
Possible effects:
- Reduced sperm motility
- Discomfort during ejaculation
- Mild obstruction of the vas deferens
- Swelling that interferes with normal sperm flow
While rare, severe pressure may worsen male fertility issues if untreated.
2. Compromised Blood Supply
If the hernia narrows or twists blood vessels entering the testicle, blood flow may be reduced. This condition, although uncommon, can negatively affect sperm production over time.
Indicators may include:
- Shrinking of the testicle (testicular atrophy)
- Dull aching or heaviness
- Lower sperm count
Blood supply issues are usually associated with large or incarcerated hernias (where tissue becomes trapped). Prompt medical treatment can prevent long-term consequences.

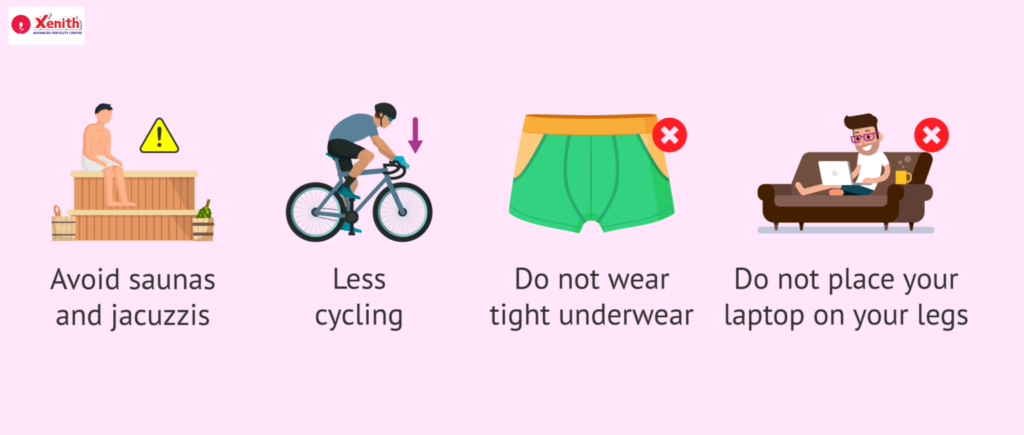
3. Increased Testicular Temperature
Healthy sperm production requires the testicles to be slightly cooler than the rest of the body. A hernia may:
- Increase warmth in the groin area
- Cause inflammation
- Lead to fluid buildup (hydrocele), which traps heat
Even small temperature increases can reduce sperm quality. While this effect isn’t universal, it helps explain why some men with untreated hernias may experience mild fertility disruptions.
Common Myths vs. Facts About Hernias and Male Fertility
Myth 1: All hernias cause infertility.
Fact: Most inguinal hernias have no direct impact on fertility. Only large, chronic, or complicated hernias pose a risk.
Myth 2: Hernia surgery always leads to infertility.
Fact: Modern hernia repair techniques are very safe. Complications involving the vas deferens or blood vessels are rare, especially with experienced surgeons.
Myth 3: If you have groin pain, your testicles are damaged.
Fact: Pain is usually due to tissue strain or nerve irritation—not damage to reproductive organs.
Myth 4: You should avoid hernia surgery if you’re planning a pregnancy.
Fact: In many cases, repairing a hernia can improve fertility by restoring normal anatomy.
Breaking these myths helps reduce anxiety and gives you clarity about your real risks.
Hernia Repair and Fertility: What You Should Know
Many men fear that hernia repair—whether open or laparoscopic—might harm the vas deferens or testicular blood vessels. This concern stems from older surgical techniques or rare surgical complications. Today’s procedures are far more refined.
How surgery affects fertility:
It often improves fertility
Repairing a hernia can:
- Remove pressure on the spermatic cord
- Restore proper blood flow
- Reduce groin inflammation and temperature
- Prevent long-term complications like atrophy
Some studies even show improved semen parameters after successful repair.
Small risk of surgical damage
The vas deferens or blood vessels may be at very small risk, especially in:
- Recurrent hernia repairs
- Large scrotal hernias
- Cases with significant scarring
Choosing an experienced surgeon is the best way to minimize this risk.
Mesh repair is generally safe
Modern mesh materials do not cause infertility. They sit outside the spermatic cord and do not interfere with sperm transport.
Diagnosing an Inguinal Hernia
If you suspect a hernia, a clinical exam is usually the first step. Your doctor may ask you to stand, cough, or strain to make the bulge more visible.
Diagnosis may include:
- Physical examination – Most hernias are diagnosed by touch.
- Ultrasound – Helpful in small or hidden hernias.
- CT scan/MRI – Rarely needed but used for complex cases.
A timely diagnosis ensures proper treatment and helps protect fertility.
Treatment Options
Not every inguinal hernia needs immediate surgery. The decision depends on your symptoms, size of the hernia, and whether it’s affecting your daily life or fertility.
1. Watchful Waiting
This approach may be suitable if:
- The hernia is small
- You have no pain or discomfort
- It doesn’t interfere with activities
- There is no evidence of pressure on the testicle
However, you’ll need regular monitoring to ensure it doesn’t worsen.
2. Surgical Repair
Surgery is recommended if:
- The hernia is growing
- You experience pain or swelling
- It interferes with exercise or sexual activity
- There are fertility concerns
- The hernia becomes trapped (incarcerated)
Types of repair:
Open repair
A small incision is made in the groin to push tissue back into place and reinforce the wall.
Laparoscopic repair
A minimally invasive technique using small holes and a camera. It often results in:
- Faster recovery
- Less pain
- Minimal scarring
Both techniques are safe and effective for most men.
When Hernia Surgery May Improve Fertility
You may actually see fertility benefits from surgery if you experience:
- Chronic pressure on the spermatic cord
- Disrupted blood flow to the testicle
- Temperature elevation due to swelling
- Pain that affects ejaculation or sexual function
Restoring normal anatomy helps the testicles function optimally again.
Lifestyle & Prevention Tips
While you cannot always prevent a hernia, you can lower the risk of worsening it—or protect fertility during recovery.
1. Preventing Worsening Hernias
- Avoid heavy lifting
- Strengthen core muscles safely
- Maintain a healthy weight
- Treat chronic cough or constipation
- Practice proper lifting techniques
These steps reduce strain on the abdominal wall.
2. Post-Surgery Recovery Tips for Fertility Safety
- Follow your surgeon’s lifting restrictions strictly
- Wear supportive underwear during recovery
- Avoid straining or heavy workouts for 4–6 weeks
- Apply ice to reduce swelling
- Report any swelling, fever, or testicular discomfort quickly
Healing well protects both the surgical repair and your reproductive health.
Most Hernias Are Treatable Without Long-Term Fertility Consequences
It’s completely understandable to worry when anything affects your groin or testicles. But the vast majority of inguinal hernias—and hernia repairs—do not cause infertility. With early diagnosis, proper care, and skilled surgical management, you can protect both your health and your fertility.
If you’re dealing with a hernia or recovering from surgery, staying informed and working closely with your doctor will help you make the best decisions for your reproductive future.